David Dodick, Wolfgang Grisold, Steven Lewis, Tissa Wijeratne
Working to promote brain health and disability.
By Tissa Wijeratne, David Dodick, Steven Lewis, Wolfgang Grisold
On World Brain Day, work continues to prevent brain disorders, diagnose brain disorders earlier, provide access to life-changing treatments and rehabilitation therapies, and improve the quality of life for those living with brain disorders with less disability and no stigma.
Health, defined by World Health Organization (WHO), is “a state of complete physical, mental, and social wellbeing and not merely the absence of disease or infirmity.”
Brain health, defined by WHO is “the state of brain functioning across cognitive, sensory, social-emotional, behavioral and motor domains, allowing a person to realize their full potential over the life course, irrespective of the presence or absence of disorders.”
Our brain health is the key to our overall health — it’s the agent for all human actions and experiences as a species.
Disorders affecting the health of our brains continue to be the leading cause of disability globally. However, many of these brain disorders can be prevented by modifying our risk factors.
For example, worldwide, around 50 million people have dementia — but nearly 50% of dementia cases can be prevented by taking steps that include maintaining a healthy weight, keeping away from smoking and too much alcohol consumption as well as learning new hobbies.
If we look at strokes, there are more than 80 million people currently living who have experienced stroke — and around 90% of those strokes could be prevented by addressing just over 10 modifiable risk factors that include things like treatment of hypertension, increased physical activity, and maintaining a healthy diet.
But there’s a lot to do to achieve these targets and save brains globally. A crucial step in changing these trends is to raise awareness of brain health.
World Brain Day was launched on July 22, 2014, as an annual, global World Federation of Neurology (WFN) advocacy campaign promoting brain health. It aims to educate everyone about the importance of keeping their brains healthy.
Every year, we focus on a different area of brain health.
This year, WFN and the World Federation of Neurorehabilitation (WFNR) have teamed up with the aim of raising awareness on brain health and disability: Leave no one behind globally.
Brain disorders such as stroke, migraine and headache disorders, dementia, head injuries, epilepsy, Parkinson’s disease, neuroinfections such as meningitis and over 400 disorders affect approximately over three billion people of all ages globally and the leading cause of disability and second leading cause of death globally.
Debilitating neurological diseases impact every aspect of a person’s life, with effects ranging from cognitive impairment to significant physical disability. Brain health-related disability will continue to increase as we continue to live longer. Raising awareness of brain health, preventative brain health is critical as we try and mitigate this issue globally.
Early diagnosis of brain disorders is important as appropriate treatment and rehabilitation programs culminating toward reduced disability. Supporting clinical research is key to the success of treating people with over 400 neurological disorders.
The past decades have shown an increase in research and many bench-to-bedside developments, which could and should be implemented in clinics around the world. Not only for the improvement and benefit of the patients, but to also change the concept of therapy in many neurological disorders radically.
By raising awareness of the treatments available and working with health care professionals around the world to recognize the signs and symptoms of neurological disorders, many more people can be diagnosed early and effectively treated.
For 2023, the WFN choose Brain Health and Disability as the theme, continuing our efforts on brain health, and aligning with WHO`s efforts to fight disability worldwide. Disability can be prevented, rehabilitated, and also needs to be under neurological care in chronic and chronic progressive diseases.
The aim of WBD 2023 is to alert not only its member societies but also the public on the critical neurological issues issue of disability. The organizing committee will represent the global regions, and we partner with the WFNR.
Member societies of the WFN will receive a “tool kit,“ templates for press releases, and educational PowerPoint presentation sets to assist in their local activity to promote WBD and advocate for brain health and disability. Local press conferences, press coverages (eg, print, electronic, radio, TV, YouTube channels) are strongly encouraged to reach the public.
Please join the World Brain Day 2023 campaign for Brain Health and Disability, as this is an important priority.
The World Federation of Neurology is hosting a global webinar on July 22, 2023, at 9 p.m. AEST with a live question-and-answer session. You can join the webinar and pre-register your interest here. •
For additional information, please see:
World Brain Day 2023 – Brain Health and Disability: “Leave no one behind.”
Wijeratne T, Dodick DW, Lewis SL, Guekht A, Pochigaeva K, Grisold W.
J Neurol Sci. 2023 Jun 29;451:120720. doi: 10.1016/j.jns.2023.120720. PMID: 37421882
The World Federation of Neurology World Brain Day 2023.
Grisold W, Dodick DW, Guekht A, Lewis S, Wijeratne T.
Lancet Neurol. 2023 Jun 29:S1474-4422(23)00240-5. doi: 10.1016/S1474-4422(23)00240-5. PMID: 37393928
Drs. Tissa Wijeratne and David Dodick are co-chairs of World Brain Day. Dr. Wolfgang Grisold is president of the World Federation of Neurology, and Dr. Steven Lewis is WFN secretary general and editor of World Neurology.












 Our job as service providers makes it our responsibility to look at the various factors that contribute to the meager medical attention received in rural areas. A deep dive into the conversations with the locals brings to light how awry education, economic constraints, and misguided prioritization contribute to this. Often the locals say, “I don’t have high blood pressure, I feel absolutely fine,” in response to showing them their chronically elevated levels, sometimes touching 200/120, or “I stopped my medications because I haven’t had a seizure in a while,” when asked why they were not compliant to medication, and sometimes, “I thought the paralysis of my face and hands were due to high sugars,” when asked why they didn’t go to the hospital for treatment. However, most times, they do have genuine reasons for not availing medical services. More often than not, their nearest hospitals are almost 100 kilometers away, which increases the time lost to treat any emergency as well as cost of travel which the family cannot bear. But of all, the most important factor would still be the lack of awareness about the disease at hand. This lack of awareness includes not knowing the symptoms of the disease, the importance of timely diagnosis and treatment, maintenance of drug compliance, complications of the disease, and how all of this will affect their livelihood. It is important because trying to eliminate this root cause empowers the people to identify their problem and take necessary steps as well as contribute to the decision making of their treatment. Once they make their first step to availing treatment, we can meet halfway to provide them with medical services.
Our job as service providers makes it our responsibility to look at the various factors that contribute to the meager medical attention received in rural areas. A deep dive into the conversations with the locals brings to light how awry education, economic constraints, and misguided prioritization contribute to this. Often the locals say, “I don’t have high blood pressure, I feel absolutely fine,” in response to showing them their chronically elevated levels, sometimes touching 200/120, or “I stopped my medications because I haven’t had a seizure in a while,” when asked why they were not compliant to medication, and sometimes, “I thought the paralysis of my face and hands were due to high sugars,” when asked why they didn’t go to the hospital for treatment. However, most times, they do have genuine reasons for not availing medical services. More often than not, their nearest hospitals are almost 100 kilometers away, which increases the time lost to treat any emergency as well as cost of travel which the family cannot bear. But of all, the most important factor would still be the lack of awareness about the disease at hand. This lack of awareness includes not knowing the symptoms of the disease, the importance of timely diagnosis and treatment, maintenance of drug compliance, complications of the disease, and how all of this will affect their livelihood. It is important because trying to eliminate this root cause empowers the people to identify their problem and take necessary steps as well as contribute to the decision making of their treatment. Once they make their first step to availing treatment, we can meet halfway to provide them with medical services. For this reason, with the goal of raising awareness as well as providing free medical services in the resource-poor and remote rural sector, a novel project “Neurology on Wheels,” a first-time project by the Dr. Bindu Menon Foundation was started in Nellore, Andhra Pradesh, India. This project identifies a village from the 46 mandals by random selection. The team of the foundation then visits the village after the village head has been informed about the camp in advance. The village sarpanch is also asked to prime the ASHA/ Anganwadi workers/ANM (local women trained to act as health educators and promoters in their communities) for efficient coordination.
For this reason, with the goal of raising awareness as well as providing free medical services in the resource-poor and remote rural sector, a novel project “Neurology on Wheels,” a first-time project by the Dr. Bindu Menon Foundation was started in Nellore, Andhra Pradesh, India. This project identifies a village from the 46 mandals by random selection. The team of the foundation then visits the village after the village head has been informed about the camp in advance. The village sarpanch is also asked to prime the ASHA/ Anganwadi workers/ANM (local women trained to act as health educators and promoters in their communities) for efficient coordination.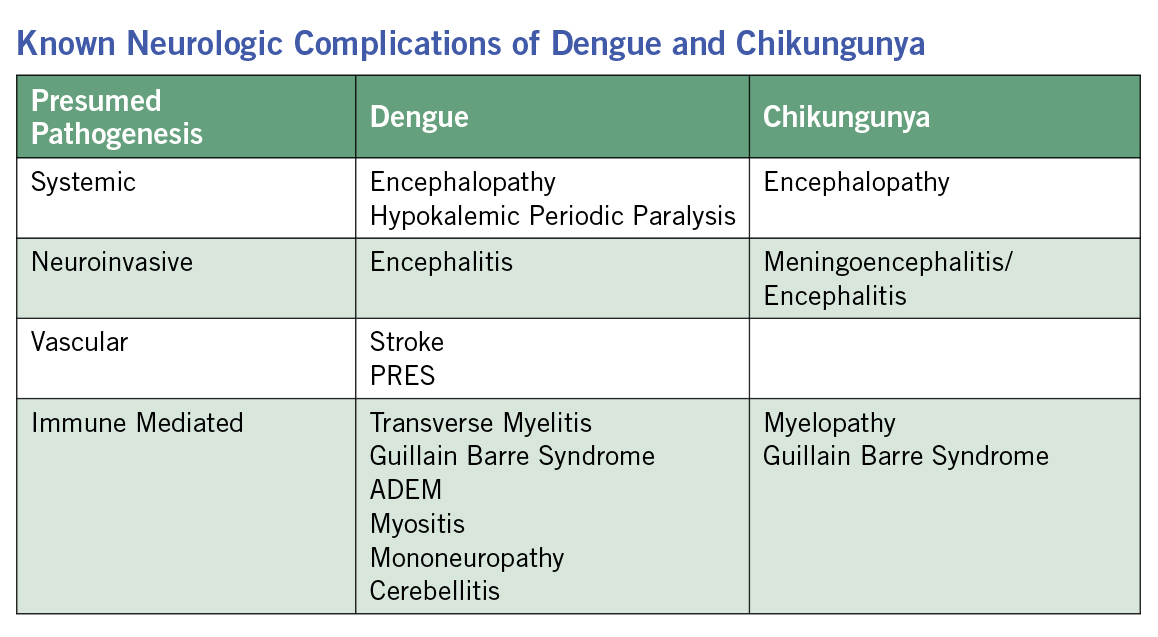 Chikungunya cases have also been increasing in early 2023, including a surge of cases in Paraguay and Brazil, with Brazil recording over twice as many cases compared to last year (
Chikungunya cases have also been increasing in early 2023, including a surge of cases in Paraguay and Brazil, with Brazil recording over twice as many cases compared to last year (