Update on several noteworthy neuroinfectious disease issues, including arboviruse as well as COVID-19 exposure in-utero.
By B. Jeanne Billioux, MD, and Avindra Nath, MD
The WHO has recently released reports denoting the expansion of cases of dengue and chikungunya beyond historical areas of transmission in the Americas, as well as warnings for increased expansion of transmission in areas of Europe that were previously unaffected (https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON448; https://www.bloomberg.com/news/articles/2023-04-05/europe-at-risk-of-dengue-and-zika-summer-outbreaks-who-warns#xj4y7vzkg). Climate change may contribute to broadening habitat for certain viral-spreading arthropods, including the Aedes aegypti mosquitoes that harbor dengue, chikungunya, and zika viruses.
Dengue has been on the rise this season, with many South American countries including Colombia, Brazil, and Argentina, as well as Asian countries, such as the Philippines, recording increased caseloads compared to prior seasons (outbreaknewstoday.com). The U.S. has also recorded several cases in Southern Florida, most of them related to travel, as well as autochthonous transmission in Maricopa County in Arizona this year (https://www.floridahealth.gov/diseases-and-conditions/mosquito-borne-diseases/_documents/2023-week14-arbovirus-surveillance-report.pdf; https://www.cdc.gov/mmwr/volumes/72/wr/mm7211a5.htm).
Dengue may present broadly, from asymptomatic cases to hemorrhagic fever; most typically, in symptomatic cases, it causes flu-like symptoms. Neurologic complications occur uncommonly, and include encephalopathy from multiorgan involvement, encephalitis, PRES, stroke (both ischemic and hemorrhagic), and immune-mediated syndromes such as transverse myelitis, Guillain-Barre syndrome, acute disseminated encephalomyelitis, myositis, mononeuropathies, and cyberelites. Some patients may develop hypokalemic paralysis (Trivedi 2022). No known treatments for Dengue exist, but several vaccines are in clinical trials or in various stages of gaining approval, including the recent approval in Brazil https://www.thepharmaletter.com/article/takeda-gains-approval-in-brazil-for-qdenga?print=1.
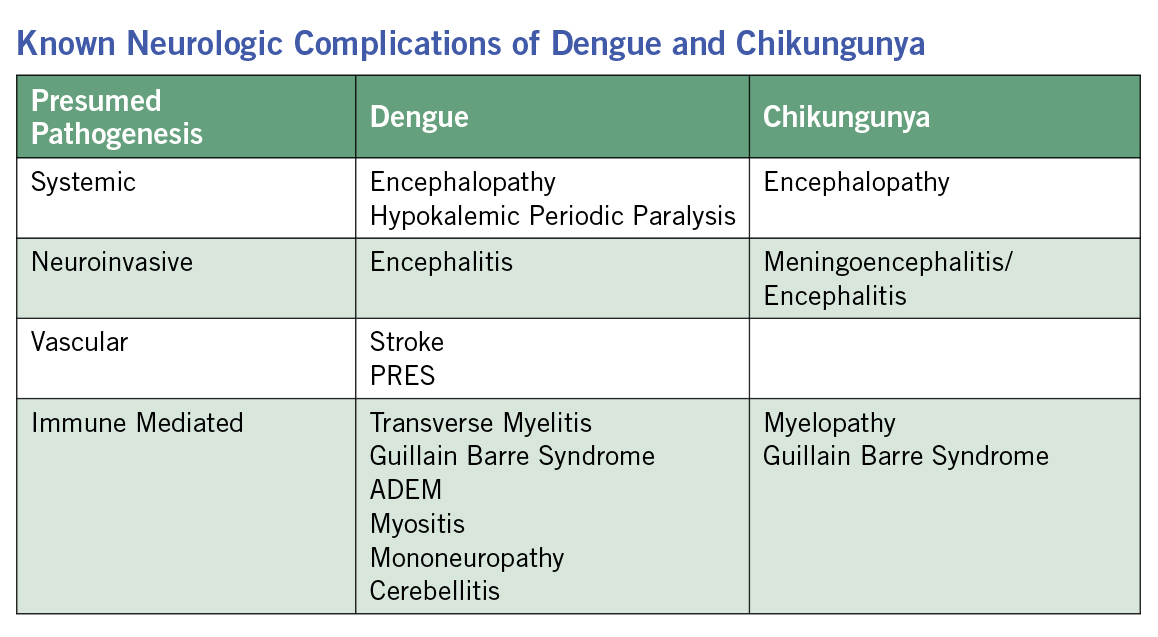 Chikungunya cases have also been increasing in early 2023, including a surge of cases in Paraguay and Brazil, with Brazil recording over twice as many cases compared to last year (http://outbreaknewstoday.com/author/news-desk/). Although the disease commonly causes fever, fatigue, malaise, and arthralgias (sometimes severe), over 200 cases of suspected meningoencephalitis have been reported due to chikungunya virus in Paraguay during this current outbreak, a rare presentation, (https://www.cidrap.umn.edu/chikungunya/paho-warns-rising-chikungunya-cases-americas-some-fatal) which needs to be closely watched since it could represent an evolution in viral tropism. Other known neurologic complications of Chikungunya include encephalopathy, encephalitis, myelopathy, and peripheral neuropathies, including Guillain-Barre syndrome (Brizzi 2017).
Chikungunya cases have also been increasing in early 2023, including a surge of cases in Paraguay and Brazil, with Brazil recording over twice as many cases compared to last year (http://outbreaknewstoday.com/author/news-desk/). Although the disease commonly causes fever, fatigue, malaise, and arthralgias (sometimes severe), over 200 cases of suspected meningoencephalitis have been reported due to chikungunya virus in Paraguay during this current outbreak, a rare presentation, (https://www.cidrap.umn.edu/chikungunya/paho-warns-rising-chikungunya-cases-americas-some-fatal) which needs to be closely watched since it could represent an evolution in viral tropism. Other known neurologic complications of Chikungunya include encephalopathy, encephalitis, myelopathy, and peripheral neuropathies, including Guillain-Barre syndrome (Brizzi 2017).
Of note, efforts to reduce transmission of dengue, chikungunya, and the neurovirulent zika virus by using Wolbachia bacteria infection in Aedes aegypti mosquitos have been underway in a number of different areas with varying levels of success. Wolbachia infection of these mosquitos essentially blocks viral replication of dengue, chikungunya, and zika in the mosquito, leading to decreased transmission of these viruses. Recent reports by the World Mosquito Program have noted decreased dengue spread in Java, Indonesia, and the Aburra Valley in Colombia, among other places, where the Wolbachia-infected mosquitos have been released (https://www.worldmosquitoprogram.org/en/learn/scientific-publications).
In COVID-19 related news, a recent case series has reported two neonates born with brain abnormalities thought to be related to in-utero exposure to SARS-CoV2. Both babies were born to mothers who had contracted SARS-CoV-2 in their second trimesters (one with re-infection during the third trimester). Both babies were SARS-CoV-2 negative at birth, but had microcephaly, seizures starting on the day of delivery, and developmental delay over time. Both infants had SARS-CoV-2 antibodies and elevated inflammatory markers, and the placenta from each case also displayed SARS-CoV-2 proteins, increased inflammatory markers, as well as evidence of decreased fetal perfusion. One infant died at 13 months of life; on autopsy, the infant was found to have white matter loss, gliosis, vacuolization, as well as evidence of SARS-CoV-2 viral proteins by immunofluorescence throughout the brain, indicating viral infection. The authors note that these two cases are extremely rare, but indicate that in-utero exposure to SARS-CoV-2 in the second trimester has the potential to cause neurodevelopmental sequelae (Benny 2023). •
References:
- Trivedi S, Chakravarty A. Neurological Complications of Dengue Fever. Curr Neurol Neurosci Rep. 2022 Aug;22(8):515-529. doi: 10.1007/s11910-022-01213-7. Epub 2022 Jun 21. PMID: 35727463; PMCID: PMC9210046.
- Brizzi K. Neurologic Manifestation of Chikungunya Virus. Curr Infect Dis Rep. 2017 Feb;19(2):6. doi: 10.1007/s11908-017-0561-1. PMID: 28233188.
- Benny M, Bandstra ES, Saad AG, Lopez-Alberola R, Saigal G, Paidas MJ, Jayakumar AR, Duara S. Maternal SARS-CoV-2, Placental Changes and Brain Injury in 2 Neonates. Pediatrics. 2023 Apr 6:e2022058271. doi: 10.1542/peds.2022-058271. https://publications.aap.org/pediatrics/article/doi/10.1542/peds.2022-058271/191033/Maternal-SARS-CoV-2-Placental-Changes-and-Brain?autologincheck=redirected