A historical sketch.
by Peter J. Koehler
Most neurologists are probably unfamiliar with the history of deep brain stimulation (DBS). Although Parkinson’s disease (PD) is probably the best-known indication, several refractory psychiatric disorders may be treated by DBS. Obsessive compulsive disorder (OCD) and depression may be mentioned with this respect. A recent dissertation from the University of Utrecht, Netherlands, by psychologist Max van der Linden shows that research in this field had already started in the 1950s.1
Somatic Therapies in Psychiatry
Several types of so-called somatic therapies may be recognized in the history of psychiatry. These evolved in a period in which neurology and psychiatry were still taught and practiced simultaneously by neuropsychiatrists in most places, except a few large cities, where it had already been split. Nobel Prize winner and Austrian Julius Wagner-Jauregg (1857-1940) started with malaria therapy for general paralysis of the insane (GPI) in the early 20th century. We already read about this in World Neurology (Volume 35, issue no. 4 of October/November 2020, pp. 5 and 10).
In the 1920s, Austrian Manfred Sakel (1900-1957) developed insulin coma therapy for schizophrenia (see World Neurology, Volume 37, issue no. 1 of January/February 2022, pp. 4-5). This was soon followed by metrazol shock therapy in the 1930s, developed by Hungarian neuropathologist/neuropsychiatrist Ladislas Meduna (1896-1964) and by electroconvulsive therapy (ECT) invented by professor of neuropsychiatry in Rome Ugo Cerletti (1877-1963) in cooperation with Lucio Bini (1908-1964) in 1938. ECT soon replaced the earlier shock therapies, as it was easier and safer to apply. Psychiatrist and historian Joel Braslow, who also included hydrotherapy and sterilization in his review of somatic therapies, reported that within a year after the introduction of ECT in the United State (1941), 42% of 356 psychiatric institutes had electroshock machines.2
Less well-known is that Roy R. Grinker (1900-1993) in Chicago also made the step from animal to human experimentally applying electricity, in this case with nasopharyngeal electrodes.3 Interestingly, he and psychoanalyst Helen V. McLean (1894-1983) tried to combine neurophysiological and psychoanalytical ideas to explain the effects of shock therapy. The core of their theory was the existence of supposed tension between the emotional biological drives in the diencephalon and the suppressive influence of the superego, believed to be located in the cerebral cortex. Blocked brain pathways were thought to be the cause of mental health symptoms. This in fact shows that the separation between the biological and psychoanalytical perspectives in psychiatry in the United States between the 1930s and 1950s was less extensive than had previously been assumed.1, p. 107-19
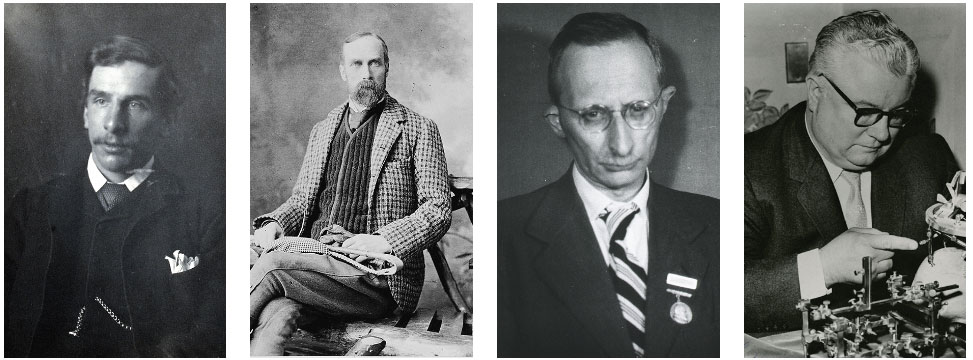
Victor Horsley (Courtesy Wellcome Institute, London). Robert Henry Clarke (Courtesy Wellcome Institute, London). Ernst A. Spiegel (Courtesy NIH, National Library of Medicine, Digital Collections). Henry T. Wycis (Courtesy NIH, National Library of Medicine, Digital Collections).
Ablative Treatments
In the meantime, the Portuguese neurologist António Egaz Moniz (18
74-1955) presented his ideas on leucotomy at the second Neurological Congress in London (1935). Frontal lobotomy was popularized by the American neurologist Walter Freeman (1895-1972) and neurosurgeon James W. Watts (1904-1994). Eventually Freeman was able to do the procedure on his own within a few minutes. Thousands of patients underwent this procedure, in particular in the U.S., England, and Scandinavia.4,5 Because of the risk of severe complications, more limited surgical procedures were being explored, including orbital undercutting, topectomy (Brodmann areas 9 and 10), and open cingulotomy.6
Although stereotactic neurosurgery had already been introduced by neurosurgeon Victor Horsley (1857-1916) and house-surgeon/ anatomist/physiologist Robert Henry Clarke (1850-1926) in 1908, their apparatus was based on skull landmarks and therefore inaccurate. It was mainly used in animal experiments.
In 1918, Canadian neuroanatomist/neuropathologist Aubrey T. Mussen (1873-1975) developed a stereotactic device for human use.7 Practice with a stereotactic device in humans only started in the 1940s, when Spiegel and Wycis used radiographic techniques, imaging landmarks like the ventricles with pneumoencephalograms (PEG) and the calcified pineal gland. In fact, the introduction in 1947 of stereoencephalotomy by originally Austrian neurologist Ernst A. Spiegel (1895-1985), who emigrated to Philadelphia in 1930, and neurosurgeon Henry T. Wycis (1911-1972) was aimed in the first place to refine leucotomy in cases of obsessions, depression, schizophrenia, and pediatric mental deficiency.6,9
“This apparatus is being used for psychosurgery. In a series of patients studied in collaboration with H. Freed [psychiatrist Herbert Freed (1908-1976)], lesions have been placed in the region of the medial nucleus of the thalamus (medial thalamotomy) in order to reduce the emotional reactivity by a procedure much less drastic than frontal lobotomy”.8 The thalamus had become the area of interest, as retrograde Wallerian degeneration in autopsied lobotomized patients pointed to this place. They later shifted their focus to movement disorders, starting with pallidoansotomies for chorea.10

(Left to right) Robert Galbraith Heath (Creative Common Licence). José M.R. Delgado (Courtesy NIH, National Library of Medicine, Digital Collections). Natalia Bechtereva (Creative Common BY 4.0). Cover of Van der Linden’s dissertation Elektrisch Evenwicht [Electic Equilibrium].
Deep Brain Stimulation (DBS) in Psychiatry
A similar motivation was given when searching for electrical stimulation methods that were less dramatic procedures than ECT. After the introduction of stereotactic neurosurgery, Heath and Delgado used this method to insert electrodes for registration as well as intermittent stimulation in these patients. Working at the department of psychiatry and neurology at Tulane University, New Orleans, psychiatrist Robert Galbraith Heath (1915-1999) was among the first to set up an interdisciplinary non-convulsive stimulation program for psychiatric patients. He started stimulating schizophrenic patients in the early 1950s and described the first 19 patients in his 1954 monograph Studies in Schizophrenia.
About the same time, neurophysiologist/neurobehaviorist José M. Delgado (1915-2011), who had moved on a grant from Madrid to Yale, was working with John F. Fulton (1899-1960), applying stimulation in the brains of animals. In 1951, he started cooperation with neurosurgeon Hannibal Hamlin (1904-1982), stimulating the frontal brain of schizophrenic patients before they underwent lobotomy. As for the animal experiments, he developed telemetric electrical stimulation for his laboratory animals so that they were able to move freely. Famous is Delgado’s experiment in the 1960s with a bull in the arena that he could stop by remote control.11 In the first years, electrodes would remain projecting from the skull, but in the 1970s following the introduction of cardiac pacemakers in late 1950s and 1960, this could be avoided by the use of subcutaneous stimulators that could deliver continuous non-convulsive stimulation.
Although many other researchers were working in this field, I will mention one more, notably the Norwegian neurophysiologist Carl Sem-Jacobsen (1921-1991), who worked at the Mayo Clinic in Rochester, Minnesota. In cooperation with neurologist Reginald Bickford (1913-1998), he initially used depth registration of epileptic and psychotic patients before selecting the site of prefrontal leucotomy. Later, they investigated the effects of stimulation and found that behavioral responses of the patients often persisted long after the stimulation. Some patients improved remarkably from the stimulation experiments.1,p.184-5
DBS for Parkinson Disease
Sem-Jacobsen eventually shifted his interest to the surgical treatment of PD applying this same technique and publishing the results in 1966. Chronic stimulation, sometimes for days or a week, was used to identify the best site for making the lesion.12 Natalia P. Bechtereva (1924-2008) presented the idea of chronic subcortical stimulation as a permanent therapy in the early 1970s and coined the term therapeutic electrostimulation. However, as implantable neurostimulators were not available in the USSR at the time, small lesions were applied.9 Several other investigators were working in the field, until the most important work by neurosurgeon Alim L. Benabid (b. 1942) and neurologist Pierre Pollak (b. 1950) in Grenoble (France) was published in 1987. In PD patients with bilateral tremor, they performed thalamotomy contralateral to the most severe tremor and carried out continuous stimulation for the other side. They concluded that “VIM [thalamic nucleus ventralis intermedius] stimulation strongly decreased the tremor but failed to suppress it as completely as thalamotomy did… This therapeutic protocol appears to be of interest for patients with bilateral extrapyramidal movement disorders”.13 Indeed, bilateral thalamotomies had important long-term adverse effects, including dysathria and ataxia.14
Concluding Remarks
We learn that human stereotactic ablation as well as electric deep brain stimulation for psychiatric diseases preceded that for movement disorders. At present, intractable OCD is the main psychiatric indication for DBS and treatment-resistant depression is a promising second indication.15 Unfortunately, Van de Linden’s dissertation Elektisch Evenwicht [Electric Equilibrium], which can be downloaded from the University of Utrecht website (Elektrisch evenwicht: Een geschiedenis van diepe hersenstimulatie bij psychiatrische stoornissen (1860-2020) (uu.nl)), was written in Dutch. However, with modern tools the pdf of the book (470 pages) can easily be read in other languages. •
Literature
1. Linden M van der. Elektrisch evenwicht. A history of deep brain stimulation in psychiatric disorders (1860-2020) [in Dutch]. Utrecht, dissertation, 2023.
2. Braslow JT. History and evidence-based medicine: lessons from the history of somatic treatments from the 1900s to the 1950s. Ment Health Serv Res. 1999;1:231-40
3. Grinker RR. A method for studying and influencing cortico-hypothalamic relations. Science. 1938;87:73-4.
4. Pressman JD. Last Resort. Psychosurgery and the Limits of Medicine. Cambridge University Press, 1998.
5. El-Hai J. The Lobotomist. Hoboken (NJ), Wiley, 2005.
6. Rzesnitzek L, Hariz M, Krauss JK. Psychosurgery in the History of Stereotactic Functional Neurosurgery. Stereotact Funct Neurosurg. 2020;98:241-247.
7. Rahman M, Murad GJ, Mocco J. Early history of the stereotactic apparatus in neurosurgery. Neurosurg Focus. 2009;27:E12
9. Spiegel EA, Wycis HT, Marks M, Lee AJ. Stereotaxic Apparatus for Operations on the Human Brain. Science. 1947;106:349-50.
10. Hariz MI, Blomstedt P, Zrinzo L. Deep brain stimulation between 1947 and 1987: the untold story. Neurosurg Focus. 2010;29:E1.
11. Marzullo TC. The Missing Manuscript of Dr. Jose Delgado’s Radio Controlled Bulls. J Undergrad Neurosci Educ. 2017;15:R29-R35.
12. Sem-Jacobsen CW: Depth-electrographic observations related to Parkinson’s disease. Recording and electrical stimulation in the area around the third ventricle. J Neurosurg 1966;24:388–402.
13. Benabid AL, Pollak P, Louveau A, Henry S, de Rougemont J. Combined (thalamotomy and stimulation) stereotactic surgery of the VIM thalamic nucleus for bilateral Parkinson disease. Appl Neurophysiol. 1987;50:344-6.
14. Dallapiazza RF, Lee DJ, De Vloo P, Fomenko A, Hamani C, Hodaie M, Kalia SK, Fasano A, Lozano AM. Outcomes from stereotactic surgery for essential tremor. J Neurol Neurosurg Psychiatry. 2019;90:474-482.
15. Borron BM, Dougherty DD. Deep Brain Stimulation for Intractable Obsessive-Compulsive Disorder and Treatment-Resistant Depression. Focus (Am Psychiatr Publ). 2022;20:55-63.