By Prof. Amadou Gallo DIOP, MD, PhD

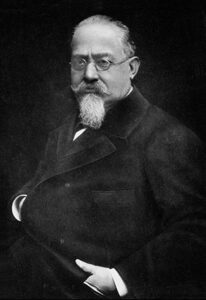
Johan Aarli
We, in Africa, definitively consider Johan Aarli as the great and generous man who, as president of WFN, put Africa on the map of world neurology. He met with Prof. Michel Dumas in 2005 at the Sydney World Congress of Neurology (WCN). Prof. Dumas is one of the first French pioneers who installed neurology in Africa, Senegal, in the late 1950s. Prof. Aarli argued that African neurologists could not be absent in the new global affairs he was leading during his World Federation of Neurology (WFN) presidency. He rapidly cemented it by inviting, for the first time, African neurology leaders to attend a business meeting at the London headquarters in 2006. He generously accepted us and listened to our dreams and goals. He set up the WFN Africa Initiative with robust, sustainable, and efficient programs of training, bursaries, and exchanges.
He traveled to Africa (the first for a WFN president) because he was curious and excited to know us better for more substantial and structured support of neurological sciences in Africa. He endorsed, with respect and high consideration, the slogan we proposed to him: “With Africa; for Africa,” which became the WCN’s slogan in Marrakech (the wonderful and first WCN in Africa) in 2011. The outcome of Prof. Aarli’s “WFN Africa Initiative” is concrete, visible, measurable, and impacting:
- Four Regional Training Centers “in Africa, for Africa” (Cairo, Cape Town, Dakar, Rabat) receiving four-year and one-year trainees from African countries with priority for the those lacking neurosciences human resources. It led to training neurologists on site, in the continent, increasing their number and combating the brain drain.
- Travel bursaries for complementary hyperspecialized training for post-doctoral African fellows to voluntary hosting sites, such as Austria, Germany, France, Italy, Norway (Prof. Aarli’s country), and Turkey.
- Strong support to regional teaching courses (RTCs) with a powerful implication of institutions such as the AAN, EAN, and others.
- Facilities and bursaries for young African neurologists for attending the WCN and other major neuroscience congresses around the world.
- The establishment of the African Academy of Neurology (AFAN), in Dakar in 2010, was a tremendous and historic administration outcome of Johan Aarli’s global initiative and legacy.
Definitively, the smiley, generous gentleman Johan Aarli will count a lot in the history of neurology in developing countries, particularly in Africa, from where we send our condolences to his extraordinary wife, Gullburg, who was with him at every WFN event around the world. Also, to his colleagues in Norway and the successive WFN staff all these last years.
Thank you, dear Johan. Africa is grateful to you. God bless you. •
Prof. Amadou Gallo is head of the Dakar WFN Regional Training Center and past WFN trustee (2013-2016)
 Johan A. Aarli was an inspiring and highly respected neurologist with a worldwide influence. Sadly, he died March 24, 2023, at age of 86 years after a long illness. He made a huge professional impact locally, nationally, and globally. Prof. Aarli was a successful president of the World Federation of Neurology 2005-2009, and a general secretary of the European Association of Neurological Societies 2003-2005.
Johan A. Aarli was an inspiring and highly respected neurologist with a worldwide influence. Sadly, he died March 24, 2023, at age of 86 years after a long illness. He made a huge professional impact locally, nationally, and globally. Prof. Aarli was a successful president of the World Federation of Neurology 2005-2009, and a general secretary of the European Association of Neurological Societies 2003-2005.
 By Kurt Niederkorn, MD, Yong-Jae Kim, MD, PhD, Hee-Jung Song, MD, PhD, and Alex Razumovsky, PhD, FAHA, NVS
By Kurt Niederkorn, MD, Yong-Jae Kim, MD, PhD, Hee-Jung Song, MD, PhD, and Alex Razumovsky, PhD, FAHA, NVS On Nov. 3-5, 2022, a joint conference of the Korean Society of Neurosonology (KSN) and NSG WFN considering clinical applications of carotid duplex, transcranial Doppler and transcranial color-coded duplex utilization in the wide arrays of different aspects of neurology, neurocritical care, and neurosurgery was conducted in Seoul, Korea. Invited speakers included prominent experts from Austria, Egypt, Germany, Japan, Korea, Portugal, Singapore, Switzerland, and the United States. Numerous speakers from Korean medical schools and universities were involved and presented high-quality clinical and research lectures.
On Nov. 3-5, 2022, a joint conference of the Korean Society of Neurosonology (KSN) and NSG WFN considering clinical applications of carotid duplex, transcranial Doppler and transcranial color-coded duplex utilization in the wide arrays of different aspects of neurology, neurocritical care, and neurosurgery was conducted in Seoul, Korea. Invited speakers included prominent experts from Austria, Egypt, Germany, Japan, Korea, Portugal, Singapore, Switzerland, and the United States. Numerous speakers from Korean medical schools and universities were involved and presented high-quality clinical and research lectures. A program full of lectures including teaching courses, hands-on sessions, poster sessions, international certification examination, and special interest events covering diverse topics, with networking and social activities, was presented. A special session was dedicated to sonography education where experts from Germany, Korea, and the United States exchanged opinions and presented country-specific approaches to neurosonology and ultrasound education in medical schools. However, the wide application of ultrasound, including neurosonology across many medical specialties, increased portability and decreased cost of ultrasound devices, and enhancement of learning both basic and clinical sciences with ultrasonography will continue to demand appropriate teaching and training on ultrasound in undergraduate medical education.
A program full of lectures including teaching courses, hands-on sessions, poster sessions, international certification examination, and special interest events covering diverse topics, with networking and social activities, was presented. A special session was dedicated to sonography education where experts from Germany, Korea, and the United States exchanged opinions and presented country-specific approaches to neurosonology and ultrasound education in medical schools. However, the wide application of ultrasound, including neurosonology across many medical specialties, increased portability and decreased cost of ultrasound devices, and enhancement of learning both basic and clinical sciences with ultrasonography will continue to demand appropriate teaching and training on ultrasound in undergraduate medical education. A special issue of the Korean Journal of Neurosonology and Neuroimaging (JNN) published all lectures and presentations (JNN, volume 14, supplement 2, November 2022).
A special issue of the Korean Journal of Neurosonology and Neuroimaging (JNN) published all lectures and presentations (JNN, volume 14, supplement 2, November 2022). Neurosonology has been developed based on ultrasound diagnosis in cerebrovascular diseases, like ischemic stroke and extracranial and intracranial stenosis, but is currently being applied and used clinically in various fields ranging from diagnosis and monitoring of cerebral vasospasm after subarachnoid hemorrhage and traumatic brain injury, and cerebral degenerative diseases, and to diagnose and follow up on peripheral nerve and muscle diseases.
Neurosonology has been developed based on ultrasound diagnosis in cerebrovascular diseases, like ischemic stroke and extracranial and intracranial stenosis, but is currently being applied and used clinically in various fields ranging from diagnosis and monitoring of cerebral vasospasm after subarachnoid hemorrhage and traumatic brain injury, and cerebral degenerative diseases, and to diagnose and follow up on peripheral nerve and muscle diseases.
 Welcoming speeches to the participants were given by Prof. Saltanat Kamenova, president of KNANN; Prof. Zhanna Kalmataeva, dean of the faculty of medicine and health at al-Farabi KazNU; Aizhan Sadykova, president of the National Medical Association; and Symbat Abzalieva, deputy director of the Higher School of Medicine at al-Farabi KazNU. They noted the special significance of the forum for all practitioners who took part in this event.
Welcoming speeches to the participants were given by Prof. Saltanat Kamenova, president of KNANN; Prof. Zhanna Kalmataeva, dean of the faculty of medicine and health at al-Farabi KazNU; Aizhan Sadykova, president of the National Medical Association; and Symbat Abzalieva, deputy director of the Higher School of Medicine at al-Farabi KazNU. They noted the special significance of the forum for all practitioners who took part in this event. The speakers of the Forum were Prof. Valery Feigin (New Zealand), Prof. Natan M. Bornstein (Israel), Prof. Adnan Siddiqui (U.S.), Prof. Afshin Divani (U.S.), Prof. Mesoud Ashina (Denmark), Prof. Tatyana Negrich (Ukraine), Prof. Aksel Siva (Turkey), as well as doctors from Kazakhstan: Saltanat Kamenova, Bagyzhan Syzdykova, Korlan Saduakasova, Tatiana Kaimak, Maksharip Martazanov, Aigul Akimniyazova, Gulnar Kabdrakhmanova, Karlygash Kuzhibaeva, and Aida Kondybaeva.
The speakers of the Forum were Prof. Valery Feigin (New Zealand), Prof. Natan M. Bornstein (Israel), Prof. Adnan Siddiqui (U.S.), Prof. Afshin Divani (U.S.), Prof. Mesoud Ashina (Denmark), Prof. Tatyana Negrich (Ukraine), Prof. Aksel Siva (Turkey), as well as doctors from Kazakhstan: Saltanat Kamenova, Bagyzhan Syzdykova, Korlan Saduakasova, Tatiana Kaimak, Maksharip Martazanov, Aigul Akimniyazova, Gulnar Kabdrakhmanova, Karlygash Kuzhibaeva, and Aida Kondybaeva. Within the framework of the forum, there was a master class titled, “Evidence-Based Neurology. How to Search for Information to Answer Specific Clinical Questions, Interpret and Critically Evaluate Scientific Evidence.” This training course was organized for young doctors and discussed the basic concepts and tools of evidence-based medicine, as well as their application in clinical and scientific practice. The course was conducted by doctors Maurizio Leone (Italy), Luca Vignatelli (Italy), Katina Aleksovska (Macedonia), and Teia Kobulashvili (Austria). •
Within the framework of the forum, there was a master class titled, “Evidence-Based Neurology. How to Search for Information to Answer Specific Clinical Questions, Interpret and Critically Evaluate Scientific Evidence.” This training course was organized for young doctors and discussed the basic concepts and tools of evidence-based medicine, as well as their application in clinical and scientific practice. The course was conducted by doctors Maurizio Leone (Italy), Luca Vignatelli (Italy), Katina Aleksovska (Macedonia), and Teia Kobulashvili (Austria). •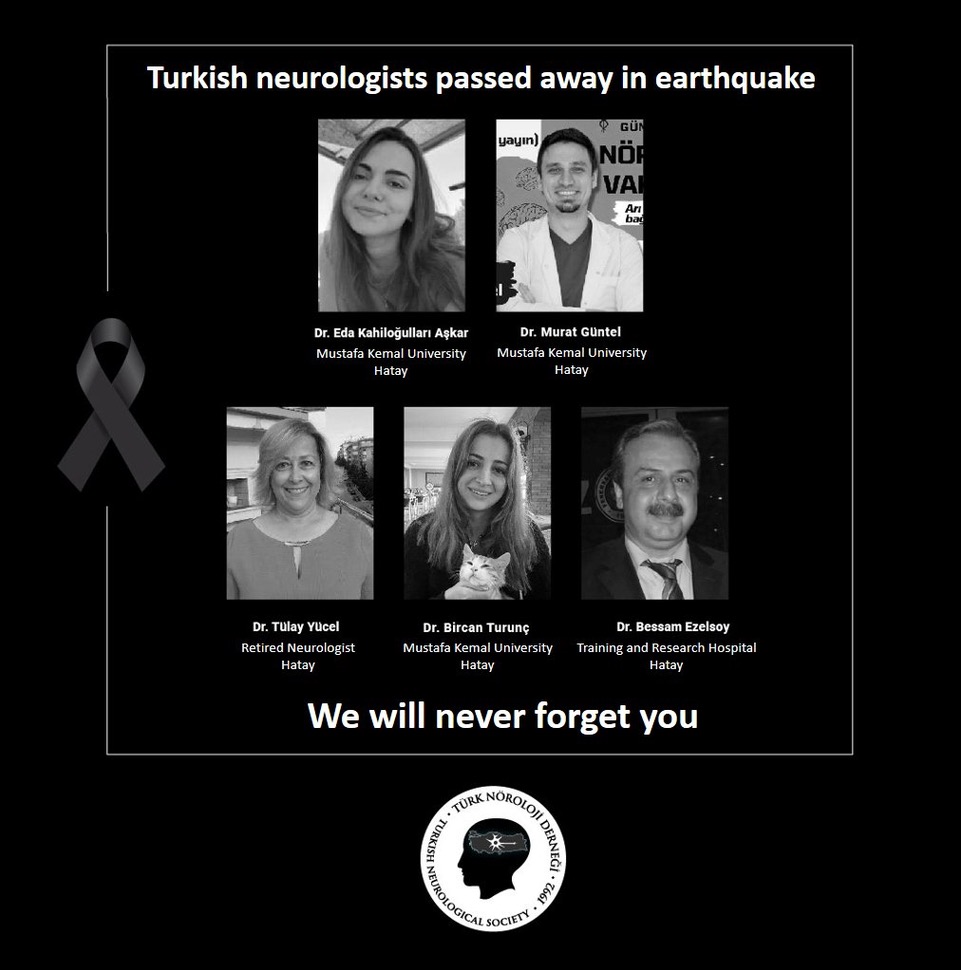 On Feb. 6, 2023, two major earthquakes occurred, nine hours apart, with epicenters in Gaziantep and Kahramanmaraş in Turkiye. In this disaster, called the 2023 Turkiye-Syria earthquakes,” nearly 43,000 people died in Turkiye and 6,000 people in Syria. A total of approximately 150,000 people were injured, of which 120,000 were in Turkiye. It is estimated that at least 3 million people migrated from the affected zone to different cities after the earthquakes. Aftershocks still continue and pose a serious risk for rescue teams. Earthquakes affected 13.5 million Turkish people in an area of 1,000 square kilometers. This refers to about one-seventh of Turkiye’s population.
On Feb. 6, 2023, two major earthquakes occurred, nine hours apart, with epicenters in Gaziantep and Kahramanmaraş in Turkiye. In this disaster, called the 2023 Turkiye-Syria earthquakes,” nearly 43,000 people died in Turkiye and 6,000 people in Syria. A total of approximately 150,000 people were injured, of which 120,000 were in Turkiye. It is estimated that at least 3 million people migrated from the affected zone to different cities after the earthquakes. Aftershocks still continue and pose a serious risk for rescue teams. Earthquakes affected 13.5 million Turkish people in an area of 1,000 square kilometers. This refers to about one-seventh of Turkiye’s population.




 World Brain Day 2023 annually commemorates the foundation of the World Federation of Neurology (WFN) on July 22. The previous World Brain Day themes focused on specific neurological diseases such as Parkinson’s disease, migraine, epilepsy, multiple sclerosis, and many others. We are again partnering with all six regions of the WFN as well as the World Federation for NeuroRehabilitation (WFNR) to unite the world on the disability that results when brain health compromised.
World Brain Day 2023 annually commemorates the foundation of the World Federation of Neurology (WFN) on July 22. The previous World Brain Day themes focused on specific neurological diseases such as Parkinson’s disease, migraine, epilepsy, multiple sclerosis, and many others. We are again partnering with all six regions of the WFN as well as the World Federation for NeuroRehabilitation (WFNR) to unite the world on the disability that results when brain health compromised. The World Stroke Congress (WSC) is the flagship meeting of the World Stroke Organization (WSO). After the exclusively virtual events in 2021 and in 2020 (joint conference with the European Stroke Organization), the WSC 2022 in Singapore was the first international large-scale in-person meeting. With more than 4,400 attendees (approximately half in person and half online) this was the largest WSC ever. It served as an excellent opportunity to discuss latest clinical and research results with colleagues from all over the world. The participants were from 106 countries with highest attendance from colleagues from Australia, China, India, Indonesia, Malaysia, Philippines, Singapore, United Kingdom and the United States. The faculty of 204 invited speakers were well balanced across continents (Asia 34%, South and North America 24%, Europe 25%, Australia and Africa 18 %).
The World Stroke Congress (WSC) is the flagship meeting of the World Stroke Organization (WSO). After the exclusively virtual events in 2021 and in 2020 (joint conference with the European Stroke Organization), the WSC 2022 in Singapore was the first international large-scale in-person meeting. With more than 4,400 attendees (approximately half in person and half online) this was the largest WSC ever. It served as an excellent opportunity to discuss latest clinical and research results with colleagues from all over the world. The participants were from 106 countries with highest attendance from colleagues from Australia, China, India, Indonesia, Malaysia, Philippines, Singapore, United Kingdom and the United States. The faculty of 204 invited speakers were well balanced across continents (Asia 34%, South and North America 24%, Europe 25%, Australia and Africa 18 %). Pacific Stroke Organization, Association of Southeast Asian Nations Neurological Association, and WHO South-East Asia Regional Office. Stroke support organizations substantially contributed to the WSC 2022, integrated into the main program and also in parallel independent sessions. During the coffee breaks, there was dialogues on non-communicable diseases (NCD).
Pacific Stroke Organization, Association of Southeast Asian Nations Neurological Association, and WHO South-East Asia Regional Office. Stroke support organizations substantially contributed to the WSC 2022, integrated into the main program and also in parallel independent sessions. During the coffee breaks, there was dialogues on non-communicable diseases (NCD). Patients with indications of endovascular stroke therapy according to DAWN or DEFUSE-3 criteria were also not considered. Other highlights were the meta-analysis of six trials comparing endovascular stroke therapy alone against bridging (combined with intravenous thrombolysis). In this meta-analysis including 2314 patients, endovascular stroke therapy could not prove to be non-inferior to bridging therapy and this is also valid for multiple subgroups. The first phase 3 trial on stem cells in stroke recovery (TREASURE) was negative, a lowering of systolic blood pressure under 120 in successful endovascular stroke therapy has negative impact on the patients’ outcome (ENCHANTED2), and treatment by tenecteplase was non-inferior to alteplase treatment (AcT Study).
Patients with indications of endovascular stroke therapy according to DAWN or DEFUSE-3 criteria were also not considered. Other highlights were the meta-analysis of six trials comparing endovascular stroke therapy alone against bridging (combined with intravenous thrombolysis). In this meta-analysis including 2314 patients, endovascular stroke therapy could not prove to be non-inferior to bridging therapy and this is also valid for multiple subgroups. The first phase 3 trial on stem cells in stroke recovery (TREASURE) was negative, a lowering of systolic blood pressure under 120 in successful endovascular stroke therapy has negative impact on the patients’ outcome (ENCHANTED2), and treatment by tenecteplase was non-inferior to alteplase treatment (AcT Study).
 The I Latin American Course of Neuroepidemiology took place in Panama City, Panama, in April 2018. This II course was initially planned to take place in March 2020. Unfortunately, the COVID pandemic forced the organizers to postpone it until 2023. The structure and the content of these Latin American courses are based on the experience of the Erice’s International Course of Neuroepidemiology. (See World Neurology, posted Feb. 24, 2023. Report on the Ninth International Course of Neuroepidemiology: Methods and Clinical Applications worldneurologyonline.com).
The I Latin American Course of Neuroepidemiology took place in Panama City, Panama, in April 2018. This II course was initially planned to take place in March 2020. Unfortunately, the COVID pandemic forced the organizers to postpone it until 2023. The structure and the content of these Latin American courses are based on the experience of the Erice’s International Course of Neuroepidemiology. (See World Neurology, posted Feb. 24, 2023. Report on the Ninth International Course of Neuroepidemiology: Methods and Clinical Applications worldneurologyonline.com). As apparent from the title, the present book by Simon Shorvon, The Idea of Epilepsy. A Medical and Social History of Epilepsy in the Modern Era (1860-2020), begins approximately, where Owsei Temkin (1902-2002) ended, although there is some overlap, in particular with respect to Bénédict Morel (1809-1873), Wilhelm Griesinger (1817-1868), Jules Falret (1824-1902), and Théodore Herpin (1799-1865), who are mentioned in both books.
As apparent from the title, the present book by Simon Shorvon, The Idea of Epilepsy. A Medical and Social History of Epilepsy in the Modern Era (1860-2020), begins approximately, where Owsei Temkin (1902-2002) ended, although there is some overlap, in particular with respect to Bénédict Morel (1809-1873), Wilhelm Griesinger (1817-1868), Jules Falret (1824-1902), and Théodore Herpin (1799-1865), who are mentioned in both books.