A Medical and Social History of Epilepsy in the Modern Era (1860-2020), Simon D. Shorvon, Cambridge University Press
By Peter J. Koehler
“Diseases can be considered as acts or invasions by gods, demons, or evil spirits, and treated by the invocation of supposedly supernatural powers. Or they are considered the effects of natural causes and are consequently treated by natural means. In the struggle between magic and the scientific conception, the latter has gradually emerged victorious in the western word. The fight has been long and eventful, and in it epilepsy held one of the key positions. Showing both physical and psychic symptoms, epilepsy more than any other disease was open to interpretation both as a physiological process and as the effect of spiritual influences.” — Owsei Temkin, 1945
The Falling Sickness
These are the first sentences in Owsei Temkin’s classic book The Falling Sickness. A History of Epilepsy from the Greeks to the Beginnings of Modern Neurology. First published in 1945, a revised edition appeared in 1971, and in 1994 it was published again. The book begins with the “sacred disease” in antiquity, discusses ancient medical science, and touches upon magic, superstition, possession, and lunacy in the Middle Ages. It then passes through the Renaissance period with the “theological debate” on possession and witchcraft, describes theoretical ideas on epilepsy in the great systems (including iatrochemistry, iatromechanics, and animism), discusses the Enlightenment, including pathology and nosology, and then enters into the nineteenth century. Here Temkin dwelt on reflex therapy, described some of the important “Jackson forerunners,” including Richard Bright (1789-1858) and Louis-François Bravais (1801-1843), whose name is sometimes eponymized in the term Bravais-Jacksonian epilepsy. The book ends with an extensive description of the ideas of John Hughlings Jackson (1835-1911) in the second half of the nineteenth century.
 As apparent from the title, the present book by Simon Shorvon, The Idea of Epilepsy. A Medical and Social History of Epilepsy in the Modern Era (1860-2020), begins approximately, where Owsei Temkin (1902-2002) ended, although there is some overlap, in particular with respect to Bénédict Morel (1809-1873), Wilhelm Griesinger (1817-1868), Jules Falret (1824-1902), and Théodore Herpin (1799-1865), who are mentioned in both books.
As apparent from the title, the present book by Simon Shorvon, The Idea of Epilepsy. A Medical and Social History of Epilepsy in the Modern Era (1860-2020), begins approximately, where Owsei Temkin (1902-2002) ended, although there is some overlap, in particular with respect to Bénédict Morel (1809-1873), Wilhelm Griesinger (1817-1868), Jules Falret (1824-1902), and Théodore Herpin (1799-1865), who are mentioned in both books.
The Authors
Temkin and Shorvon have quite different backgrounds. Temkin was born in Minsk (in the present Belarus) and received his MD from the University of Leipzig (1927), where he was in contact with well-known medical historians like Henry E. Sigerist (1891-1957) and Karl Sudhoff (1853-1938). Following his MD, he worked at the Leipziger Medizinhistorischen Institut. Both Sigerist and Temkin emigrated to the U.S. (Johns Hopkins University, Baltimore) in 1932 and Temkin remained a medical historian. Some of his important books are Galenism: Rise and Decline of a Medical Philosophy (1973) and Hippocrates in a World of Pagans and Christians. Shorvon, on the other hand, has a background in clinical medicine. He is an emeritus professor of clinical neurology at the University College of London (UCL) Queen Square Institute of Neurology and Hon. Consultant Neurologist at the National Hospital for Neurology and Neurosurgery. In the latter hospital, he specialized in epilepsy. He published books not only on epilepsy, but also on the history of neurology, including ILAE [International League Against Epilepsy] 1909-2009, A Century of History (2009), Physicians at War (2016), 500 Years of the Royal College of Physicians (2018), and the acclaimed Queen Square. A History of the National Hospital and its Institute of Neurology (in cooperation with Alastair Compston; 2019).
The Idea of Epilepsy
These two books by Temkin and Shorvon complete a fantastic review of the history of epilepsy. Whereas Temkin’s 1994 edition on the early history of epilepsy comprised 488 pages, Shorvon’s new book on the 1860-2020 period has as many as 750 pages. The latter book contains a wealth of information about the latest 160 years, in which knowledge of epilepsy increased tremendously. In the introduction, the author appropriately uses the metaphor of a ship named “Epilepsy” sailing through the long twentieth century. Very appropriately, he is aware that the medical and scientific aspects of the history of epilepsy are not the only that need to receive attention. A disease such as epilepsy in particular has many important aspects that deserve to be addressed. Therefore, the author chose to examine the history of epilepsy from four perspectives, not only including the medical and scientific, but also the societal and personal perspective. Furthermore, he tried not just to answer the question, “What happened?” but also “why it happened,” the latter of course being much more difficult and even “hazardous.”
The reason why he chose to begin in 1860 is that he considered this the period of the first modern conceptions of epilepsy. Indeed, the mid-nineteenth century was the period in which medicine definitely became based upon science. This was related to August Comte’s (1798-1857) positivistic philosophy. Scientific knowledge was obtained by representing results in measure and number. Claude Bernard (1813-1878) and Rudolf Virchow (1821-1902) were important proponents of the scientific method in medicine. Their respective books Introduction à l’étude de la médecine expérimentale (CB 1865) and Die Cellularpathologie in ihrer Begründung auf physiologische und pathologische Gewebelehre (RV 1858) may be considered milestones of the scientific method in medicine.
Epilepsy and Psychiatry
The 160 years that are discussed in Shorvon’s book are divided into five periods:
1. 1860-1914 (“The birth of modern epilepsy”)
2. 1914-1945 (“Epilepsy in the age of catastrophe”)
3. 1945-1970 (“Epilepsy and the new world order”)
4. 1970-1995 (“Epilepsy in a globalized world”)
5. 1995-2020 (“The epilepsy floods are too recent”)
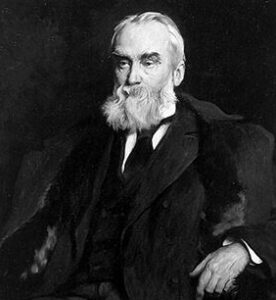
Cesare Lombroso (courtesy Wellcome Collection)
In each period, the four mentioned perspectives pass in review. The relationship between epilepsy and psychiatry in the first mentioned period is intriguing. The author mentions Cesare Lombroso’s (1835-1909) and his famous book L’uomo delinquente (1876), in which the author focused on the link between epilepsy and crime. Furthermore, Shorvon stated that “it was in the context of the study of mental symptoms in epilepsy that the theory of dégénérescence (degeneration) was proposed, again by Morel,” referring to his 1857 Traité des dégénérescences physiques, intellectuelles et morales de l’espèce humaine et des causes qui produisent ces variétés maladives [A treatise on the physical, intellectual and moral degenerations of the human species and the causes that produce these morbid varieties]. Indeed, Morel published on the relationship between epilepsy and his degeneration concept, but it was in a number of articles in the Gazette hebdomadaire that he described his concept of épilepsie larvée (masked epilepsy).1 The degeneration concept started in psychiatry with proponents such as Morel and Valentin Magnan (1835-1916).
“Insanity gradually came to be considered a brain condition and a product of degeneration rather than a psychological disorder. … A ‘taint’ or sickly deviation from the norm initially caused by a pathogenic environment, poor nutrition, or alcoholic abuse, and subsequently transmitted in the Lamarckian manner through heredity, becoming progressively more severe with each generation until the family line became sterile and, finally, extinct”.2
Later in his career (1880s), Jean-Martin Charcot (1825-1893) believed that heredity also played an important role in neurological conditions and thought these afflictions could be interrelated by means of inheritance.3 It is of interest to mention that the degeneration concept had a tremendous impact on the fin de siècle society, including its literature. In one of his lectures, he said, “Gentlemen, I will now present for clinical examination, two unfortunate creatures who deserve compassion. One may say that one as well as the other have been touched by the antique fatality that nowadays has been substituted by hereditary fatality.”
Among other fictional characters, Shorvon provides the example of Emile Zola’s (1840-1902) La Bête Humaine, in which a character carried “the physical stigmata of epilepsy.” In fact, the concept of degeneration can be found in the whole 20-volumes Rougon-Macquart series. It should be realized that the fin de siècle was characterized by cultural malaise partly caused by these ideas of degeneration, but also by the uncertainty and anxiety of approaching the end of a century. Fear for decay and disaster reigned. The notion of degeneration was perceived by the lay public as well as by artists.3,4
An interesting section is dedicated to “psychoanalytic theory and epilepsy.” The author tells us that psychoanalysis provided a novel explanation of epilepsy. “As its theories matured, the view grew that essential epilepsy was the result of inhibited psychological development caused by inherited traits which prevented normal psychic development and were manifest both by epileptic seizure and abnormalities of personality” (p. 166). Indeed, it is a general phenomenon that new ideas and therapies in medicine initially have a much broader area of indications, to become much narrower or disappearing after some time. As for neurology, another affliction in which this happened, i.e. psychotherapy, was dystonia.5 A few other issues of interest discussed here are the idea of the epileptic personality and the psychiatric effects of temporal lobe epilepsy.
Stigma
Fjodor Dostoievsky (public domain)
Shorvon dedicates a paragraph on “eugenics and epilepsy.” Indeed, it did not escape involuntary sterilization in some countries, not just in Nazi Germany in the 1930s and 1940s. Furthermore, it is fascinating to read about the early pathophysiological ideas, including the reflex theory, the idea of autointoxication, and the Bacillus epilepticus (1916). And, of course, he mentions the asylums and colonies established for epileptic patients, in a period when drugs where less successful than today. The stigma of having epilepsy and the patient’s experience are discussed in detail. Several celebrities are mentioned in the context, like Queen Victoria’s epileptic son Prince Leopold of Albany and the Russian writer Fjodor Dostoievsky (1821-1881). He not only suffered from epilepsy himself, but also wrote about it in several of his novels. Although it is not certain, he may have been treated by the optimistic Herpin. He was one of the doctors Dostoevsky listed on his visa application of 1863, the year in which he traveled abroad for the official purpose of consulting the greatest European authorities on epilepsy, including Moritz Romberg (1795-1873), Armand Trousseau (1801-1867), and Herpin. It is likely Dostoevsky had Herpin in mind when writing The Idiot.6,7
The importance of the introduction of the EEG (1929) and the early twentieth-century drugs are all mentioned in the book, including those that have disappeared later. A paragraph is dedicated to the role of the pharmaceutical industries through history. A table on the chemical and physiological basis of neurotransmission between 1900 and 1970 is also provided. Several “new” pictures can be seen in the book, like the one of Horsley in the operating theatre with Samuel A. Kinnier Wilson (1878-1937) and Emil T. Kocher (1841-1917), c. 1906.
Why not Brown-Séquard?
Charles-Edouard Brown-Séquard (public domain)
Although it is impractical to include all historical texts dealing with epilepsy, I would have expected a more extensive discussion of Charles-Edouard Brown-Séquard (1817-1894) and his views on epilepsy. Having written my dissertation on Brown-Séquard’s localization concept, I am of course biased, but in the present book only a sentence and two footnotes are dedicated to him. I was surprised all the more so, since he was in fact the predecessor of Shorvon himself. After all, considered an expert in epilepsy, Brown-Séquard was the one of the founder-physicians to be appointed at the National Hospital for the Paralyzed and Epileptic (1859), where he became a teacher of Hughlings Jackson. Jackson’s colleague and life-long friend Jonathan Hutchinson (1828-1913) wrote: “My friend fell, soon after he joined me in London life, under the influence of Dr. Brown-Sequard, who told him strongly that it was foolish to waste his efforts in wide observation of disease in general, and that if he wished to attain anything he must keep to the nervous system.”
John Hughlings Jackson (public domain)
Furthermore, it was Brown-Sequard who told Hughlings Jackson that a vacancy for the post of assistant physician would be advertised. He indeed applied and was appointed on in May 1862.8 Brown-Séquard was among the first to prescribe bromide for epilepsy9, pp. 102-14 and between 1850 and 1872 published many articles as well as a book on epilepsy.10 Furthermore, he had found an experimental model for what he called spinal epilepsy, which became also known as Brown-Séquard’s epilepsy.11,12
Finally, from today’s perspective, it is doubtful whether it was truly an epileptic phenomenon, as it was related to the ankle clonus by Wilhelm Heinrich Erb (1840-1921) and Charcot. However, it aroused interest for several decades.9, pp.183-93 Perhaps Shorvon did not discuss him, because it was partly before 1860, although the same is true for Herpin and his book Du pronostic et du traitement curatif de l’épilepsie [Prognosis and treatment of epilepsy] that was published in 1852. Or perhaps it is due to the fact the Brown-Séquard’s concept was finally rejected as epilepsy in the sense of having its origin in cortical cells.
Neurosis
I may be in error, but sometimes I wondered whether the author sufficiently distinguished between the old neurosis concept and the modern post-Freudian term (psycho)neurosis. On page 58, we find that “epilepsy was still viewed generally as a mental disorder in the period under consideration, and treated largely in the arena of psychiatry.” It is of importance to understand the history of the term neurosis, as its meaning underwent an important evolution, which is related to neurology as well as psychiatry.13 William Cullen (1710 – 1790) of Edinburgh coined the term neurosis, applying it to what his Edinburgh colleague and predecessor Robert Whytt (1714-1766) called nervous diseases. This functional orientation of neurosis remained during almost the whole nineteenth century,14 though the category of neuroses became smaller as more diseases were found to have a neuropathologic substrate, beginning with general paralysis of the insane in the 1820s. In the 1880s, for example, William Gowers (1845-1915) mentioned the following functional disorders: chorea, paralysis agitans, tremor, tetanus, tetany, occupation neurosis, etc.15
During the twentieth century, even more of these neuroses were found to have an organic basis. The present sense of the term neurosis dates from the period of dynamic psychiatry in the beginning of the twentieth century and may be called psychoneurosis, e.g. anxiety neurosis, obsessional neurosis, etc. Interestingly, neurologists have treated these patients with “nervous disorders” or “nerves” for a long period.16,17 Therefore, I am not sure whether the old concept of neurosis can be equated with mental disorder, as it was associated rather with the fact that no pathological substrate was found. As for the “arena of psychiatry,” we have to realize that in many countries, particularly the German-speaking and those adopting the German system, neurology was included in psychiatry for several decades.
Criticism
The author is to be lauded that he tried to write not only for physicians, neurologists in particular, but wished to write also for the “informed public.” Therefore, he included a glossary of technical terms. Furthermore, he tried to avoid making it a book on “Great Men” and find a balanced choice with respect to the level of details. Indeed, the book is not based on important physicians in the field of epilepsy.
One shortcoming, which the author mentions himself in the introduction, is that there is a bias of language. He examined texts mainly in English. That does not mean, by the way, that he does not mention French and German researchers, but I suppose he often will have used existing translations for that purpose. And indeed, he does describe important players in the field of epilepsy from other countries than England and the United States.
Perhaps among the minor criticisms the fact could be mentioned that the author often refers to the Pitié-Salpêtrière hospital. The “new” Pitié hospital (where Joseph Babinski [1857-1932] worked since 1895), however, was built near the Salpêtrière only in 1911 and the merging of the two took place in 1964. And Paul Broca of course did not show that “the expression of speech was localized in the left frontal gyrus in 1871” (p. 74). He localized it in the frontal convolution in 1861 and only in the 1863-5 period, he realized that most cases were in the left hemisphere. Furthermore, we read “The first systematic studies of anatomical-topographical analysis using electrical stimulation were by Fritsch and Hitzig.” Indeed, they found positive results of their cortical stimulation experiments in 1870, however, in the early nineteenth century, many other experimenters preceded them, without seeing any limb movements. As medical historian Michael Hagner wrote: “These results were repeatedly reproduced by distinguished physiologists like François Magendie, François-Achille Longet, Carlo Matteucci, Julius Budge, and Moriz Schiff, and, moreover, these physiologists failed in attempts to evoke muscle twitching through cortical stimulation, whether with electrical stimulation, cauterization, or compression.” And I am not sure whether the experiments by Fritsch and Hitzig were really more systematic than the previous. Continuing in Hagner’s article “Several divergent paths led to the emergence of this stimulus experiment. They led through realms of clinical medicine that had nothing to do with localized diseases of the brain, through therapeutic practices, and not least through alternate experiments and theories that arose from entirely other lines of questioning.”19
The End of Epilepsy?
Perhaps, in a book on the history of a certain subject, one would not expect to continue the story up to the present. On the other hand, in this book on epilepsy, the story is told by an experienced epileptologist, who was part of that story for 40 years. Therefore, it is obvious that he provides his own opinion in the Epilogue, where he writes: “Even if fascinating in its own right, any history of epilepsy can be useful only if it helps make sense of the reality of epilepsy today” (p. 585), although he realizes and explains, in the accompanying footnote, that history can only stimulate new thinking about the present.
It would be a mistake to think that events in history and today are homologous, referring to philosopher Hannah Arendt (1906-1975). Using the appropriate metaphor of epilepsy as ideas, “like leaves, seeming strong and vigorous at one time, wither and fall with a transience and an insignificance unthinkable at the time,” the author states that the tree also has permanent structures like branches and a trunk that grow. Indeed, he also attempted to make up an “epilepsy balance sheet” with theories and practices that have improved or harmed epilepsy through the long twentieth century. In the accompanying text, he contemplates about what happened and what deserves criticism in the various fields, including the political and economic context, legislation and social attitude, delivery of epilepsy healthcare, pharmaceutical attitude, etc. An interesting paragraph in the Epilogue is “The harm caused by medicine.”
In the introduction and Epilogue again, Shorvon tries to answer the question, whether “Epilepsy really exists” today, or stated differently “The end of epilepsy?” Hereby he follows up on Temkin, who titled the final section of his book “The end of the falling sickness.” May it still be considered a disease, as in the past, or did the progress in knowledge result in disappearance of the disease, now only being a symptom (pp. 7 and 623)?
From the medical and scientific perspective there are, Shorvon believes, numerous arguments to drop the term epilepsy as a disease and continue to use epileptic seizure as a clinical manifestation or symptom. Referring to the German neurologist/medical historian and émigré Walther Riese (1890-1976), he realized that epilepsy is not just a medical and scientific concept, but also an idea laden with social and personal signification. Thinking of the disadvantages of the stigma, the author concludes: “Given that it does not exist as a disease, that it carries with it dark and deeply engrained archetypal memories of heredity, mental disease and impairment, and that it confers prejudice and social exclusion, I think the removal of the term ‘epilepsy’ from public discourse is at least worthy of debate. My personal opinion is that the gain might well outweigh the drawbacks. Much as Temkin had hoped, perhaps at this juncture, the end of epilepsy is possible to envisage. This would indeed be a goal worth achieving” (p. 629).
In conclusion, this book is a rich source of interesting aspects of the history of epilepsy in the past 160 years. It is recommended for physicians, in particular neurologists, and those non-medically trained persons interested in epilepsy and its history. •
References:
- Lund M. On Morel’s ‘épilepsie larvée: the first Danish epileptologist Frederik Hallager’s opposition in 1884 against Morel’s psychical epileptic equivalents. J Hist Neurosci. 1996;5:241-53.
- Goldstein J. Psychiatry. In: Bynum WF, Porter R, eds. Companion encyclopedia of the history of Medicine. London, Routledge, 1997.
- Koehler P. About medicine and the arts. Charcot and French literature at the fin-de-siècle. J Hist Neurosci. 2001;10:27-40.
- Koehler PJ. Charcot, la salpêtrière, and hysteria as represented in European literature. Prog Brain Res. 2013;206:93-122.
- Munts AG, Koehler PJ. How psychogenic is dystonia? Views from past to present. Brain. 2010;133:1552-64
- Johnson BR. Diagnosing Prince Myshkin. The Slavic and East European Journal 2012;56:377-93.
- Rice JL. Dostoevky’s Medical History: Diagnosis and Dialectic. The Russian Review. 1983;42:131-61.
- Critchley M, Critchley EA. John Hughlings Jackson. Father of Englsih Neurology. New York, Oxford University Press, 1998, pp. 37-8.
- Aminoff MJ. Brown-Séquard. An Improbable Genius Who Transformed Medicine. New York, Oxford University Press, 2011.
- Brown-Séquard CE. Researches on epilepsy. Its artificial production in animals and its etiology, nature and treatment in man. Boston: Clapp, 1857
- Koehler PJ. Brown-Séquard’s spinal epilepsy. Med Hist. 1994;38:189-203.
- Koehler PJ. Het localisatieconcept in de neurologie van Brown-Séquard. Amsterdam, Rodopi, 1989, pp. 59-63.
- López Piñero JM. Historical origins of the concept of neurosis. Cambridge: University Press, 1983.
- Bynum WF. The nervous patient in eighteenth- and nineteenth-century Britain: the psychiatric origins of British neurology. In: Bynum WF, Porter R, Shepherd M, editors. The anatomy of madness. Vol.1, , London, Tavistock, 1985, pp.89-102.
- Gowers WR. A manual of diseases of the nervous system. 2 vols. London, Churchill, 1886-1888.
- Shorter E. A history of psychiatry. New York, Wiley, 1997, pp.113-144.
- Koehler PJ. Development of neurology as a specialty in Europe. In: Education Program Syllabus: History of neurology, American Academy of Neurology, 2007, pp. 72-89
- Philippon J, Poirier J. Joseph Babinski : A Biography. New York, Oxford University Press, 2009, pp. 151-66.
- Hagner M. The electrical excitability of the brain: toward the emergence of an experiment. J Hist Neurosci. 2012;21:237-49.
