By Dr. Chandrashekhar Meshram

Chandrashekhar Meshram
The Tropical and Geographical Neurology Specialty Group of the World Federation of Neurology, in collaboration with the Forum for Indian Neurology Education (FINE), organized a neuroinfection webinar series held every Saturday from July 18 to Sept. 5. It was first educational activity of its kind by a WFN specialty group. The event was formally inaugurated by Prof. Raad Shakir, immediate past president of the WFN and chair of the WFN specialty groups, in the presence of WFN Secretary General Prof. Wolfgang Grisold. The series was dedicated to Prof. Jagjit Singh Chopra. In the last session, tribute was paid to the late Prof. Amilton Barreira, who was secretary general of the specialty group. Dr. Chandrashekhar Meshram, president of the Tropical and Geographical Neurology Specialty Group of the WFN, was the course director.
Talks were given by Hector Garcia on neurocysticercosis, by Erich Schmutzhard on cerebral malaria, by Marco Tulio Medina on Zika and other arbovirus infections, by Riadh Gouider on neurobrucelloisis, by Serefnur Ozturk on encephalitis, by Jeremy Day on cryptococcal meningitis, by Prof. Avindra Nath on the approach to neurologic infections, and by Prof. Joseph Berger on fungal meningitis.
Interesting and challenging cases of dengue, rabies, Japanese encephalitis, leprosy, tuberculous myelitis, CJD, neurocysticercosis, amoebic encephalitis, HIV, SSPE, neurobrucellosis, strongyloidosis, JC virus granule cell neuronopathy, cryptococcal infection in the immunocompromised host, histoplasmosis, antiphospholipid antibody syndrome, cerebral venous sinus thrombosis, aspergillosis, scrub typhus myositis, neurosyphilis, listeria encephalitis, mucormycosis, and H1N1 encephalitis were presented and discussed during the series. The complexities in manifestations, course, and treatment in different cases were the highlights of the series. There were analytical interactions from the faculty and audience.
Sarosh Katrak, S.Prabhakar, John England, Gustavo Roman, Chris Kennard, Wolfgang Grisold, Hadi Manji, Deanna Saylor, Steven Lewis, Kiran Thakur, Davis Garcia-Azorin, B. S. Singhal, Augustina Charway-Felli, JMK Murthy, Marianna de Visser, and Jacques Reis chaired the sessions.
Participants were from different countries across the globe, and more than 1,400 delegates registered for the series. Regular participants were from India, Sri Lanka, Bangladesh, Pakistan, Brazil, Peru, Honduras, South Africa, Ghana, Kuwait, UAE, Sudan, Zambia, and the United States. Participants interacted with the faculty through question and answer sessions.
Reports of the sessions were published in Indian newspapers as part of public education activities.
Those who missed live attendance at the sessions can watch the videos on YouTube, the links to which are available on the WFN website. https://wfneurology.org/2020-09-10-wfn-fine
Second Neuroinfection Series Happening Now
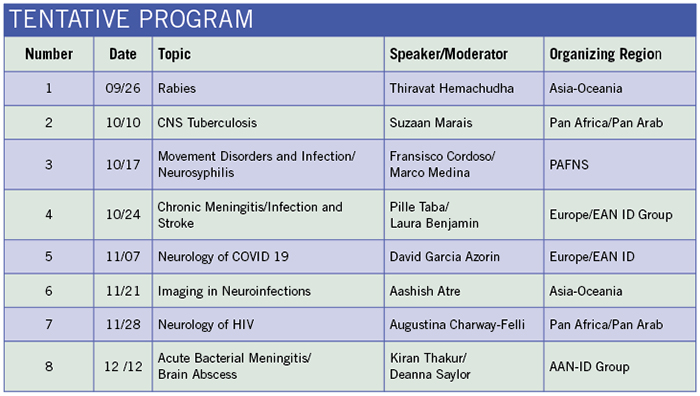
Encouraged by the success of this series, the Tropical and Geographical Neurology Specialty Group, in collaboration with Indian Academy of Neurology and FINE, planned the second WFN Neuroinfection series with eight sessions that began on Sept. 26. WFN President Prof. William Carroll inaugurated this second series. Organization of the sessions rotated between Asia-Oceania, PAFNS, the AAN ID group, Europe-EAN ID group, and the Pan Africa and Pan Arab regions. Those interested in presenting cases should contact the respective moderator for the session.
Registration is free. Link for registration can be found at: https://forms.gle/BX3xyKcztAWzLGyu6
Registered delegates will be informed about the details of the session by email before each session.
Link to join the program: https://us02web.zoom.us/j/87248087732
Password: wfnni
Each session takes place at 1 p.m. GMT/UTC and can also be watched on YouTube.
We encourage delegates from different countries participate and present the cases.•