A Cautionary Tale From the History of Malaria Fever Therapy
By Aernoud T.L. Fiolet and Ingrid M. Daey Ouwens
Introduction
History is the present seen through the eyes of the future. Now, more than ever, we are confronted with this aphorism, as one of the most impressive contemporary pandemics unrolls. As of mid-October 2020, according to the WHO (https://www.who.int/emergencies/diseases/novel-coronavirus-2019), more than 39 million cases have been confirmed worldwide, including more than 1 million deaths. The societal and economic sequelae of the virus management are felt on a global scale. Meanwhile, scientific research on the subject has surged. Fundamental research quickly provided insight on the virus genome and its systemic dissemination.1 Many institutions and pharmaceutical industries have reallocated resources on the development of therapeutic solutions. The focus is on effective vaccination, strategies to reduce the hyperinflammatory response, and support of the critically ill.2,3 While attempting to catalyze the process of resolving current unmet needs, the risks of compromising scientific integrity and validity may become apparent.4
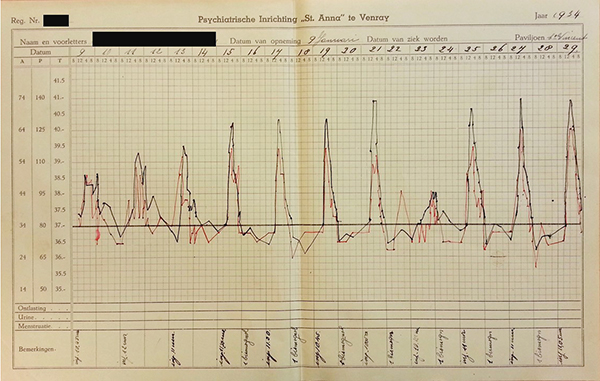
A chart of a patient with General Paralysis of the Insane, dated 1954. The points and connecting curves depict the three-day cycle of recurrent fever after inoculation with Plasmodium vivax, paralleled by an increase in heart rate.
The history of medicine teaches us that the elusive nature of a disease and the urgency felt by the medical society to treat it may incite as well as impede scientific development. An example par excellence is the intentional inoculation with plasmodium, the causative agent of malaria, to induce fever in patients suffering from General Paralysis of the Insane. In the early 20th century General Paralysis of the Insane was a much feared and nearly always lethal presentation of syphilitic infection. Future Nobel prize laureate Julius Wagner-Jauregg evoked a paradigm shift for the treatment of this condition when he developed malaria fever therapy.5
This paper on the introduction of malaria fever therapy for General Paralysis of the Insane aims to provide a meaningful insight into pitfalls that may arise during scientific developments in urgent times, then and now.
General Paralysis of the Insane and Malaria Fever Therapy
General Paralysis of the Insane, also designated “General Paralysis” or “dementia paralytica,” caused a worldwide health care problem with a considerable social and economic impact during the turn of the 19th to 20th century. At its peak, one-fifth of admissions and one-third of deaths in asylums in western Europe and the United States were attributable to General Paralysis of the Insane.6 In this tertiary form of syphilis, progressive neurological and psychiatric symptoms occurred six months to several decades after the initial syphilitic infection. Most patients died within six years after diagnosis. Various applications of highly toxic heavy metals, e.g. mercury, sulphuric acid, and arsenic acid, were used to treat early stages of syphilis, mostly with some success. As with all manifestations of syphilis, long-term treatment was required, hence the expression, “One night in the arms of Venus leads to a life on Mercury.” However, these methods were of limited use in General Paralysis of the Insane.7
Beneficial effects of fever due to an intercurrent disease in patients with somatic and psychiatric conditions have been reported since classical times.8 The Austrian psychiatrist Julius Wagner-Jauregg (1857-1940) took this approach one step further by intentionally inducing fever in psychiatric patients.8,5 At the end of the 19th century, he started his experimental treatments using streptococci, tuberculin, and typhoid vaccine. The results, however, were disappointing. He continued this line of research more than a decade later. In 1917, he induced fever by inoculation of blood containing plasmodium. The ensuing malarial fever spikes were terminated with quinine bisulphate. In addition, the patients received neosalvarsan, an arsenic, to treat their syphilitic infection. This treatment, referred to as malaria fever therapy, was adopted as the standard treatment for General Paralysis of the Insane by the global scientific community within 10 years of Wagner-Jauregg’s first report.9
Contemporary Scientific Report on Malaria Fever Therapy
Wagner-Jauregg’s first report comprised a case series of 10 malaria-inoculated patients with General Paralysis of the Insane. Nine of these patients contracted malaria. Following this treatment, two patients showed permanent considerable improvement with regard to General Paralysis of the Insane, four patients suffered relapses, two had to be sent to an asylum, and one patient died.5
Gerstmann, at the time an assistant at Wagner-Jauregg’s clinic, reported that at the end of 1921 more than 200 patients had been treated with malaria fever therapy in their clinic, of whom 50 had been able to return to work. These results encouraged the introduction of malaria fever therapy not only in Europe, but also in South America and the USA. In 1926, an international review of 2,460 cases recorded in the literature found that 27.5% of the treated patients improved greatly and another 25.6% moderately in accordance with the findings of Gerstmann.10 In 1927, Wagner-Jauregg was awarded the Nobel Prize in Physiology or Medicine “for his discovery of the therapeutic value of anti-malaria vaccination in the treatment of dementia paralytica.” This recognition undoubtedly contributed at an international level to an increase in the number of malaria fever treatments applied. Within 10 years of Wagner-Jauregg’s first report, malaria fever therapy was globally adopted as the standard treatment for General Paralysis of the Insane.9
Current Appraisal of Malaria Fever Therapy
The reported treatment outcome appeared very favorable for a previously considered untreatable condition. However, the evidence to support the efficacy of malaria fever therapy was weak. It is remarkable that in 1933 malaria fever therapy was not yet subjected to a standardized set of regulatory research criteria, while at that time any drug used in the treatment of patients was controlled with formal standards including animal research, toxicity tests, histopathological studies, tests of therapeutic efficacy, and approval by a federal regulatory board.9 Only observational studies were available with many differences in often poorly described patient characteristics and diagnostic criteria. By 1924, malaria fever therapy was also used in asymptomatic individuals who had a positive Wassermann reaction (indicating syphilitic infection), in order to prevent the development of late stage General Paralysis of the Insane.8,9 The number of patients included is often not clarified. Differences in malarial strains used, the mode of infecting the patient (inoculation of malaria-infected blood versus the bite of infected mosquitoes), number of fever spikes left untreated, pharmacological treatments preceding or following malaria fever therapy, and outcome criteria will all have influenced the results.9 Moreover, differentiation between treatment outcome and spontaneous remission requires a long follow-up period of at least three years, much longer than the usual follow-up period reported in the studies.
Perhaps most importantly, it was not possible to isolate the effect of the induced fever in itself from the effect of concomitant heavy metal therapy and general hygiene strategies taken to improve the patient’s general health. Fresh air, good nutrition, massage, hydrotherapy, and the elimination of physical and mental stress were implemented in the hope of increasing the bodily defense against the syphilitic infection and to strengthen the condition of the patients prior to the exhausting effects of malaria fever therapy.7,9
Lastly, reporting bias may have led to a distortion of the published results. Wagner-Jauregg and Gerstmann did not report the death of three out of four newly inoculated patients with General Paralysis of the Insane in 1917 or 1918. Due to Wagner-Jauregg’s omission to microscopically examine blood prior to inoculation, these patients had received blood containing plasmodium vivax. As he later documented in his memoirs, these patients consequently had contracted malaria tropica, a malignant form of malaria.5 p136 When he resumed his “vaccination” trials later in 1920, Wagner-Jauregg only used blood taken from cases of confirmed tertian malaria. Risks associated with malaria fever treatment were considerable, with reported mortality rates varying from 4% to 20%.7 The relatively high morbidity and mortality rates concomitant with this severe form of treatment seem to have received initially a mostly perfunctory discussion, probably as a result of the general feeling of hopelessness in patients and physicians with regard to General Paralysis of the Insane. As Moore, professor of Medicine at The Johns Hopkins University, whose whole professional career was devoted to the study and treatment of syphilis, put it: “desperate situations usually justify desperate risks”.9
In conclusion: the history of malaria fever therapy teaches us that a compelling need to contribute to the solution of a global health problem may compromise critical appraisal; in this example the situation led to the introduction of a globally applied and Nobel Prize-awarded treatment of uncertain benefit. Therefore, even in the midst of a pandemic, it is necessary to find the right balance between the rapid availability of therapeutic and preventive measures on the one hand, and careful research and ethical considerations on the other. •
REFERENCES
- Shang, J., Ye, G., Shi, K., Wan, Y., Luo, C., Aihara, H., Geng, Q., Auerbach, A., & Li F. (2020). Structural basis of receptor recognition by SARS-CoV-2. Nature, 581, 221-224. https://doi.org/10.1038/s41586-020-2179-y
- Callaway E., Cyranoski D., Mallapaty S., Stoye E., & Tollefson J. (2020) The coronavirus pandemic in five powerful charts. Nature, 579, 482-483.
- The RECOVERY Collaborative Group.(2020) Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report. New England Journal of Medicine. doi/10.1056/NEJMoa2021436
- Mehra M. R., Desai, S. S., Kuy, S., Henry, T. D., & Patel, A. N. (2020). Retraction: Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19. N Engl J Med. DOI.10.1056/NEJMoa2007621
- Wagner – Jauregg J (1936) Fieber- und Infektionstherapie: ausgewählte Beiträge 1887 – 1935 mit verknüpfenden und abschließenden Bemerkungen, p12, 117-138, Verlag für Medizin, Weidmann & Co. Wien, Leipzig, Bern.
- Daey Ouwens, I.M., Lens, C. E., Fiolet, A.T.L., Ott, A., Koehler, P. J., & Verhoeven, W. M.A. (2015). Clinical presentation of General Paralysis of the Insane in a Dutch psychiatric hospital, 1924-1954. European neurology, 74(1-2), 54-59. doi.org/10.1159/000435835
- Daey Ouwens I.M., Lens C.E., Fiolet A.T.L., Ott A., Koehler P.J., Kager P.A., & Verhoeven W.M.A.. (2017) Malaria Fever Therapy for General Paralysis of the Insane: A Historical Cohort Study. European Neurology, 78, 56-62. doi.org/10.1159/000477900
- Whitrow, M. (1990). Wagner-Jauregg and fever therapy. Medical history, p12, 34(3), 294-310. DOI: https://doi.org/10.1017/S0025727300052431
- Warren, J. R. (2000). A critical history of the malaria fever therapy of general paresis. Thesis University of Calgary. doi:10.11575/PRISM/23211
- Brown E.M. (2000) Why Wagner-Jauregg won the Nobel Prize for discovering malaria therapy for general paresis of the insane. History of Psychiatry 9: 371–382. doi.org/10.1177/0957154X0001104403
