Prof. Grisold reviews the impact of the Global Burden of Disease (GBD) update, brain health, and World Brain Day.
Wolfgang Grisold

Prof. Wolfgang Grisold delivering his address on brain health at the Camera dei Deputati in Rome.
I welcome you to the new edition of World Neurology, the newsletter of the World Federation of Neurology (WFN). It contains information about the WFN, and reports and publications from members and invited individuals. World Neurology is free to download from the WFN website, and the World Neurology archive is a valuable source of information on many aspects of neurology. World Neurology is entirely sponsored by the WFN, has no other support, and is not subject to any outside influences.
The Global Burden of Disease
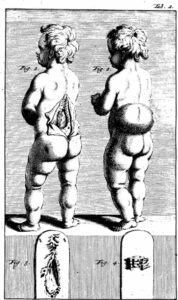
The release of the new version of the GBD will have a strong impact on the neurological community [Collaborators 2024]. It enlarges the spectrum of neurological conditions from 15 to 37, and includes other disease entities and disciplines, which are affected by neurological symptoms and often disability. See an overview in these infographics.
I was privileged to add a comment to the new release of the GBD (Grisold 2024).
One example of many includes neonatal birth injury, where the neurological sequelae are not an immediate effect for neurology, but are inevitable during the life course of the individual. This example and several others will expand the need for neurological structures and services, and come in a timely manner to align with the efforts of the WHO Brain Health Unit in regard to Brain Health and the Intersectoral Global Action Plan (IGAP). The IGAP and the Toolkit are advancing under the leadership of the WHO, and its overall effect on all aspects of neurology will be tremendous (Grisold et al. 2023).
By choosing the words “all aspects” of neurology, I mean that not only the scientific field of neurology and neuroscience, but all concerned, such as persons with lived experiences and health care professionals. Importantly, the public and the policymakers are also important stakeholders.

Figure 1: Prioritizing brain health: Awareness and public interest must be promoted.
Brain Health
The process of inserting “brain health” in the agenda of neurological societies, and in the further process on political agendas, is important. In addition to the European EAN efforts and the efforts of the AAN, brain health has been put on the political agendas of some countries, such as Norway, Switzerland, and recently Italy. These advances help to promote the concept of brain health, and once in a political agenda, it can be assumed that the idea and concept will be developing, surpass attention and awareness, and result in practical advances.
The implementation of brain health in the agenda of scientific societies is essential. The centerpiece is the adoption of brain health into the political agenda of a country.
After Switzerland, the most recent example of taking brain health into the political agenda is Italy, where on March 12, the Strategia Italian per la Salute del Cervello 2024-2031 was held in the Camera dei Deputati (Chamber of Deputies) in Rome, which is at the highest political level.
It was orchestrated by the Italian Society of Neurology (SIN). The importance of brain health was acknowledged, and during the meeting several Italian societies involved in neurology at all levels participated. Orazio Schillaci, the Italian minister of health, gave an inaugural speech. From the international neurology community, Prof. Paul Boon from the EAN and I (from the WFN) were invited for short speeches of introduction on the importance of brain health. Prof. Matilda Leonardi advised us on the importance of brain health for Italy and was involved in the development of the event.
My address pointed out that the WFN is actively engaged in brain health and has devoted the recent World Brain Days (WBDs) to the topic of brain health. The upcoming WBD is on brain health and prevention, following the previous WBDs on brain health, and brain health and disability. I also emphasized that within brain health, the implementation of IGAP will need increased efforts and promotion as the spectrum of persons needing neurological care is likely to increase after the release of the new GBD.
The WFN wants to congratulate SIN and Italian politics for taking up and engaging in this important matter of brain health.
Education in Neurology
Education Is one of the WFN’s core missions. We are happy to announce that the number of applications for WFN training sites, consisting of training centers and department visits, is increasing. In Africa, we currently have four training centers, and in Mexico, we have one training center.
In Africa, we have a full four-year training position in Senegal and Cape Town, and in Rabat, there is a four- year training position starting up, in addition to two neuromuscular fellowships. Since 2016, the ICNMD, a specialty group from the WFN, regularly sponsors one candidate for neuromuscular training in Africa each year from the Congress surplus. The first ICNMD virtual meeting in December was successful, and we look forward to the next ICNMD congress in Perth, Australia, which will have an exciting program concerning all aspects of neuromuscular disease.
Encouraged by our experience with the Virtual WCN 2021, the hybrid WCN in Montreal 2023, and our successful educational days with AFAN and AOAN, we will launch a two-day WFN Digital Neurology Updates (WNU) 2024 meeting. The WNU will be virtual, will take place Sept 26-27, 2024, and will consist of plenary lectures regarding the most frequent neurological conditions, followed by a series of teaching courses in the afternoon. In between the scientific parts, we will also have industry-sponsored symposia. We hope this series of update lectures will be exciting and useful, and our outreach will be as intense as it was for the WCN 2023 in Montreal.

The WNU2024 is a new initiative of the WFN.
World Brain Day 2024
The theme for World Brain Day 2024 is “Brain Health and Prevention.” It will be organized by the WBD committee and the WFN regions, and will create an attractive program to emphasize and stress the importance of brain health worldwide and selectively emphasize prevention.
Prevention is a pillar of the IGAP, and prevention in non-communicable and infectious disease is a powerful tool. This tool will help to reduce the number of neurological diseases as well as reduce the sequelae such as reduced quality of life and disability.

Wolfgang Grisold (left) and Carlos Hunt, WFN London Office, at the WFN booth at the meeting of the Austrian Society of Neurology at the Imperial Palace in Vienna.
Visit the WFN website to see the progress of development. There will be a toolbox to download material, which can be adapted and used for local promotion. We encourage all readers to use this incentive locally and celebrate WBD. We also welcome your reports from WBD celebrations, which will be potential candidates for publication in World Neurology.
Meet Us
The WFN had a booth at the meeting of the Austrian Society in Vienna and at the meeting of the American Academy of Neurology (AAN) in Denver this year.
We will have booths at the Japanese Society of Neurology in Tokyo, and at the meeting of the European Academy of Neurology (EAN) in Helsinki. If you visit any of these congresses, please visit our booth. You can also make an appointment for a meeting with our office (carlos@wfneurology.org). •
References
Collaborators, G. B. D. Nervous System Disorders. 2024. Global, regional, and national burden of disorders affecting the nervous system, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol.
Grisold, W. 2024. The expanding burden of neurological disorders. Lancet Neurol 23 (4):326-327.
Grisold, W., M. Freedman, R. Gouider, A. Guekht, S. Lewis, M. Medina, C. Meshram, G. Rouleau, R. Stark, and Neurology Trustees of the World Federation of. 2023. The Intersectoral Global Action Plan (IGAP): A unique opportunity for neurology across the globe. J Neurol Sci 449:120645.
Grisold, W., K. Karlshoej, M. Freedman, R. Gouider, A. Guekht, S. L. Lewis, M. T. Medina, C. Meshram, G. Rouleau, and R. J. Stark. 2022. Brain health as a global priority, view from WHO: Editorial from the World Federation of Neurology. J Neurol Sci 440:120337.

 Tissa Wijeratne, David Dodick, Steven Lewis, Alla Guekht, Wolfgang Grisold
Tissa Wijeratne, David Dodick, Steven Lewis, Alla Guekht, Wolfgang Grisold 





 By Salsabil Abdulrahim Mady Abulazayem
By Salsabil Abdulrahim Mady Abulazayem