With Information on the International Consortium on CVT Registry
By José M. Ferro, MD, PhD

The public and the global medical community have been exposed since early March 2021, both from the media, the official agencies, and the medical literature, to multiple and often contradictory information, concerning the risk of “uncommon” thrombosis occurring after vaccination against SARS-CoV-2. Most of the news concerned the vaccine manufactured by AstraZeneca and more recently the vaccine from Johnson and Johnson/Janssen. The uncommon thromboses were splanchnic and cerebral venous thrombosis (CVT), mostly the latter.
Mass vaccination is currently humanity’s great hope to control the pandemic. Vaccines were developed, tested, and approved in an incredibly fast pace, about one year since the onset of the pandemic. Administration of a vaccine simultaneously to millions of persons in multiple locations of the world was never done before in human history. Not surprisingly, extremely uncommon side effects of the vaccine, which were not detected in randomized trials of hundreds or thousands of subjects, can emerge when a much larger sample of millions is exposed to the vaccine.
COVID-19 Infection and CVT
CVT was known to occur as a rare complication (0.08%) of COVID-19, accounting for 4.2% of all acute cerebrovascular disease occurring during COVID-19 infection. Several case reports, case series, and systematic reviews of CVT associated with COVID-19 infection have been reported since the beginning of the pandemic 1,2. Both a systematic review2 and a large study based on administrative data from a hospital network3 indicate than the incidence of CVT increased with COVID-19 infection.
CVT can be the initial clinical manifestation of the infection, but the majority of CVTs develop within 13 days of onset of COVID-19 symptoms. Recognized risk factors for CVT are present in only one third of the patients. The main pathophysiological mechanism is related to the hypercoagulable state seen in moderate/severe COVID-19 disease. In fact, CVT patients often have very high D-Dimers, low fibrinogen levels, and low platelet counts. The prognosis is less favorable; namely case fatality (40%) is higher than the non-COVID-19 CVT (5-10%). Management is similar, namely on what concerns the use of parenteral heparin in the acute phase of CVT.
Case Reports and Case Series of CVT Occurring After Vaccination Against SARS-CoV-2
The European Medicines Agency (EMA) approved four vaccines against SARS-CoV-2: two mRNA vaccines from Pfizer and Moderna and two adenovirus vector DAN vaccines from AstraZeneca (AZ) and Johnson & Johnson/Janssen (JJ). The AZ vaccine is not yet approved for use in the United States.
Shortly after the onset of mass vaccination with those vaccines in Europe and in several other countries around the world, there were signals and thereafter publications of case reports and small case series of severe CVT occurring in young women within days of vaccination with the AZ vaccine 4-8. The growing number of those events led several countries to contraindicate the AZ vaccine in young and middle-aged adults, despite the total number of signaled cases being low (<200) as well as the estimated absolute risk of CVT (5 per million vaccinated individuals). In April, a small number of similar cases were reported in the U.S. after the JJ vaccine 9, leading the authorities to temporarily pause the use of that vaccine. A few individuals developed immune thrombocytopenia (ITP) 10 without thrombosis after receiving the mRNA vaccines. There are a few CVTs also reported, but the percentage of CVT occurring after mRNA vaccination is much smaller than for the adenovirus vector DNA vaccines
A striking feature of those cases was the high frequency of thrombocytopenia, which is uncommon in pre-COVID-19 CVT (<10% of the cases). Some other patients had only thrombocytopenia, splanchnic venous thrombosis, or hemorrhagic phenomena, or a combination of those, eventually with CVT. Although most of the emphasis has been placed in the thrombocytopenia, the most serious event, which may be fatal, is CVT. CVT is obviously also the most relevant event to the neurology community.
From the published cases and those signaled to the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC), a clinical profile of CVT associated with the AZ vaccine can be extracted:
- CVTs occur almost exclusively in women below age 60.
- Only about one third has traditional risk factors for CVT, such as thrombophilia or use of estrogenic contraceptives.
- CVT occurs up to 20 days after the administration of the first dose of the vaccine.
- A high percentage (up to two thirds) has thrombocytopenia; some have high D-Dimers and low fibrinogen.
- The clinical picture is often of a malignant CVT, with multiple sinus and veins thrombosis, cerebral hemorrhages and oedema, causing herniation, often requiring decompressive craniectomy, as a live-saving intervention.
- The mortality is high (~25%).
- Patients with traditional risk factors for CVT do not appear to have an increased risk of CVT after vaccination.
Possible Pathophysiological Mechanisms
Chance association or undetected recent COVID-19 infection are possible, but unlikely, explanations for CVT occurring after AZ and JJ vaccines. They cannot account for the different risk of CVT after each type of vaccine, not for the distinct clinical laboratory profile, as described in the previous section. Moreover, SARS-CoV-2 PCR nasopharyngeal swabs were negative in all the patients, in whom that test was performed (or reported to be performed), and patients only displayed antibodies against the virus spike protein antigen (most probably a vaccine effect) and not against other antiviral antibodies, as expected if they were recently infected.
Shortly after the notice of the first cases of venous thromboses with thrombocytopenia, a group of researchers from Germany, Ontario, and Vienna under the leadership of Andreas Greinacher identified the mechanism of the thrombotic complications of AZ vaccine, which they called “thrombotic thrombocytopenia.” Unfortunately, this label underscores the fact that the main feature of the syndrome is CVT, with the consequent risk of death and disability. Their patients tested positive on a screening platelet factor 4 (PF4)-heparin immunoassay. None of the patients had received heparin before blood for the tests was drawn. Patients also tested positive on a platelet-activation assay in the presence of PF4 independent of heparin. Platelet activation was inhibited by high levels of heparin and immunoglobulin4. They concluded that the vaccine resulted in a rare thrombotic thrombocytopenia mediated by platelet-activating antibodies against PF4, which clinically mimics autoimmune heparin-induced thrombocytopenia (HIT). In recent years, it has been recognized that triggers other than heparin (polyanionic medications, infections, surgery) can also cause a HIT-like coagulopathy, which can also be spontaneous. The pivotal observations of Greinacher et al 4 were confirmed by other researchers11. This post-vaccinial entity is now named vaccine-induced prothrombotic immune thrombocytopenia (VIPIT) or vaccine immune thrombotic thrombocytopenia (VITT).
A similar laboratory observation was found in the cases reported after the JJ vaccine. This finding raises the suspicion that the adenovirus vector could be the initial trigger of antibody production. The adenovirus vector carries negatively charged DNA, which binds to the positively charged PF4. An alternative explanation is the strong inflammatory stimulus of the vaccination or cross-reaction of antibodies produced by the vaccine and PF44. RNA is charged positively, so this immune response is unlikely to occur after mRNA vaccines.
Management of Cerebral Venous Thrombosis Occurring After Vaccination Against SARS-CoV-2
The risk of CVT following AZ vaccine being estimated as only five cases per million vaccinated people, it is evident that no randomized trials are possible to inform management decisions. Evidence comes from case series, analogy with HIT management, and expert consensus statements, and therefore is of low quality. Strong recommendations are not possible and the most sensible option is to produce guidance documents that will be periodically updated, as new evidence is produced.
Vaccinated persons should be informed that they may experience a transient headache a few days after vaccination. If the headache persists or is unusually severe, or they have any other neurological symptom, they should seek urgent medical advice. These patients should be examined by a neurologist.
If the clinical picture is suspicious of CVT, cerebral CT with venography or MR with MR venography should be performed to confirm, or not, the diagnosis of CVT. Meanwhile, a complete blood cell count and film, coagulation tests (INR, APTT, fibrinogen, D-Dimers) and COVID antibodies are obtained.
If CVT is confirmed and platelet count is below 150×109/L, VITT is a possibility. However, if the results of coagulation tests, fibrinogen, and D-Dimers are normal, VITT is unlikely, and the patient can be managed accordingly to the current CVT Guidelines12, namely be treated with low molecular or unfractionated heparin in the acute phase.
On the contrary, if any of those tests is abnormal, VITT is suspected and a HIT Elisa test (capable of detecting PF4 antibodies) should be performed. Consultation with a hematologist is advisable to guide on further testing (e.g., functional HIT assays) and discuss management. Meanwhile, platelet transfusions should be avoided, IV immunoglobulin (e.g., 1 mg/kg for 2 days) be administered, and a non-heparin anticoagulant (argatroban, danaparoid, or direct oral anticoagulants) be used instead of heparin4,11. Endovascular treatment of CVT can also be an option.
The International Consortium on CVT Initiative
From the available evidence so far, it is apparent that CVT after SARS-CoV-2 vaccines can be a heterogeneous group of patients. While most appear to have an immune mechanism (VITT), a few other cases may be coincidental, related to the usual CVT risk factors or even to recent COVID-19 infection. Therefore, a detailed analysis of non-selected CVT cases who developed after any COVID-19 vaccination needs to be performed.
The International Cerebral Venous Thrombosis Consortium (ICVTC) is an existing, global collaboration by academic researchers with the primary aim to perform investigator-initiated research on the epidemiology, manifestations, and outcome of patients with CVT.
Currently, 32 hospitals are participating in the consortium and have already collected data of 1,308 patients with CVT, prior to the COVID pandemic. ICVTC recently launched a prospective registry to report clinical manifestations, laboratory findings, management and outcome of patients with CVT after any COVID-19 vaccination. The registry will include CVT patients with radiologically confirmed CVT, with onset of CVT symptoms within four weeks of COVID-19 vaccination, and informed consent. Principal investigator is Jonathan Coutinho from the Amsterdam University Medical Centers (j.coutinho@amsterdamumc.nl).
Conclusion
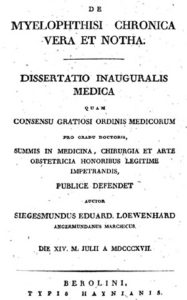
Medicine should follow the ethical principle of “Primum non nocere” (first do not harm). However, ethics should also be applied with justice. We must consider that the individual risk of CVT following COVID infection is much higher (6x) than that following any anti-SARS-CoV-2 vaccine3, even without considering the indirect effect of the infection through contagium. Therefore, the fundamental message for the public should focus on the urgent need, safety, and confidence on vaccines.
Epidemiological, clinical, and laboratory research will unveil the multiple remaining unanswered questions on the occurrence of CVT after anti-SARS-CoV-2 vaccines. Meanwhile, neurologists and other health care workers must be aware of this very rare complication of the AZ and JJ vaccines. Management of the occasional CVT patient occurring after those vaccines should follow the most recent guidance statements from national13 and international official agencies and from scientific societies14, which are likely to be updated as evidence grows. Inclusion of those cases in the ongoing International Consortium on Cerebral Vein Thrombosis registry is welcome. •
From the Serviço de Neurologia, Centro Hospitalar Lisboa Norte; J Ferro Lab, Instituto de Medicina Molecular João Lobo Antunes, Faculdade de Medicina, Universidade de Lisboa; Lisboa, Portugal. jmferro@medicina.ulisboa.pt
Inclusion Criteria for the International Consortium on CVT Registry
Patients with cerebral venous thrombosis with:
- Radiologically confirmed CVT
- Onset of CVT symptoms within 4 weeks of any COVID-19 vaccination
- Informed consent, according to local law
For more information, contact Dr. Jonathan Coutinho at j.coutinho@amsterdamumc.nl.
References
-
Dakay K, Cooper J, Bloomfield J, Overby P, Mayer SA, Nuoman R, Sahni R, Gulko E, Kaur G, Santarelli J, Gandhi CD, Al-Mufti F. Cerebral Venous Sinus Thrombosis in COVID-19 Infection: A Case Series and Review of The Literature. J Stroke Cerebrovasc Dis. 2021 Jan;30(1):105434. doi: 10.1016/j.jstrokecerebrovasdis.2020.105434
-
Baldini T, Asioli GM, Romoli M, Carvalho Dias M, Schulte EC, Hauer L, Aguiar De Sousa D, Sellner J, Zini A. Cerebral venous thrombosis and severe acute respiratory syndrome coronavirus-2 infection: A systematic review and meta-analysis. Eur J Neurol. 2021 Jan 11:10.1111/ene.14727. doi: 10.1111/ene.14727
-
Taquet M, Husain M, Geddes JR, Luciano S, Harrison PJ. Cerebral venous thrombosis: a retrospective cohort study of 513,284 confirmed COVID cases and a comparison with 489,871 people receiving a COVID-19 mRNA vaccine. In press
-
Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination. N Engl J Med. 2021 Apr 9. doi: 10.1056/NEJMoa2104840
-
Castelli GP, Pognani C, Sozzi C, Franchini M, Vivona L. Cerebral venous sinus thrombosis associated with thrombocytopenia post-vaccination for COVID-19. Crit Care. 2021 Apr 12;25(1):137. doi: 10.1186/s13054-021-03572-y
-
Schultz NH, Sørvoll IH, Michelsen AE, Munthe LA, Lund-Johansen F, Ahlen MT, Wiedmann M, Aamodt AH, Skattør TH, Tjønnfjord GE, Holme PA. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination. N Engl J Med. 2021 Apr 9. doi: 10.1056/NEJMoa2104882
-
Mehta PR, Mangion SA, Benger M, Stanton BR, Czuprynska J, Arya R, Sztriha LK. Cerebral venous sinus thrombosis and thrombocytopenia after COVID-19 vaccination – a report of two UK cases. Brain Behav Immun. 2021 Apr 12:S0889-1591(21)00163-X. doi: 10.1016/j.bbi.2021.04.006
-
Muir K-L, Kallam A, Koepsell SA, Gundabolu K. Thrombotic Thrombocytopenia after Ad26.COV2.S Vaccination. N Engl J Med. 2021 Apr 14. doi: 10.1056/NEJMc2105869.
-
Franchini M, Testa S, Pezzo M, Glingani C, Caruso B, Terenziani I, Pognani C, Bellometti SA, Castelli G. Cerebral venous thrombosis and thrombocytopenia post-COVID-19 vaccination. Thrombosis Research (2021), https://doi.org/10.1016/j.thromres.2021.04.001
-
Lee EJ, Liu X, Hou M, Bussel JB. Immune thrombocytopenia during the COVID-19 pandemic. Br J Haematol. 2021 Apr 14. doi: 10.1111/bjh.17457
-
Scully M, Singh D, Lown R, Poles A, Solomon T, Levi M, Goldblatt D, Kotoucek P, Thomas W, Lester W. Pathologic Antibodies to Platelet Factor 4 after ChAdOx1 nCoV-19 Vaccination. N Engl J Med. 2021 Apr 16. doi: 10.1056/NEJMoa2105385.
-
Ferro JM, Bousser MG, Canhão P, Coutinho JM, Crassard I, Dentali F, di Minno M, Maino A, Martinelli I, Masuhr F, Aguiar de Sousa D, Stam J; European Stroke Organization European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis – endorsed by the European Academy of Neurology. Eur J Neurol. 2017 Oct;24(10):1203-1213. doi: 10.1111/ene.13381
-
Pai M, Grill A, Ivers N, et al. Vaccine-induced prothrombotic immune thrombocytopenia VIPIT following AstraZeneca COVID-19 vaccination: lay summary. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;1(16). https://doi.org/10.47326/ocsat.2021.02.16.1.0
-
Oldenburg J, Klamroth R, Langer F, Albisetti M, von Auer C, Ay C, Korte W, Scharf RE, Pötzsch B, Greinacher A. Diagnosis and Management of Vaccine-Related Thrombosis following AstraZeneca COVID-19 Vaccination: Guidance Statement from the GTH. Hamostaseologie. 2021 Apr 1. doi: 10.1055/a-1469-7481



 We are also soliciting nominations of the names for WFN medals for 2021 ( https://wfneurology.org/activities/education-grants-and-awards/wfn-awards ).
We are also soliciting nominations of the names for WFN medals for 2021 ( https://wfneurology.org/activities/education-grants-and-awards/wfn-awards ).








 Let us spread the key messages from WBD 2021: Stop Multiple Sclerosis through mainstream media, social media platforms, and local, regional, national and international meetings throughout the year. Please see and share our new logo, the web banners, social media images, and other educational material in your country. We invite our readers to rally around WBD 2021 with the aim to stop multiple sclerosis.
Let us spread the key messages from WBD 2021: Stop Multiple Sclerosis through mainstream media, social media platforms, and local, regional, national and international meetings throughout the year. Please see and share our new logo, the web banners, social media images, and other educational material in your country. We invite our readers to rally around WBD 2021 with the aim to stop multiple sclerosis.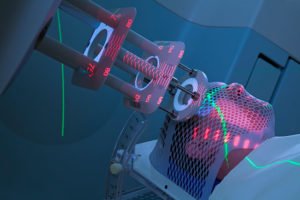 Cancer is one of the most important conditions in human health, and due to longer life expectation and improved therapies, survival in cancer patients is also increasing. This has several implications in the management of cancer patients as the longer survival changes the “natural” course of many tumors.
Cancer is one of the most important conditions in human health, and due to longer life expectation and improved therapies, survival in cancer patients is also increasing. This has several implications in the management of cancer patients as the longer survival changes the “natural” course of many tumors.



