EAN Congress
By Syrine Ben Mammou
 Thanks to World Federation of Neurology, I had the opportunity to attend the Eighth European Academy of Neurology Congress June 25-28, 2022, in Vienna Austria.
Thanks to World Federation of Neurology, I had the opportunity to attend the Eighth European Academy of Neurology Congress June 25-28, 2022, in Vienna Austria.
Since the COVID-19 pandemic, many conferences were cancelled or presented virtually. This was my first participation in an international congress of neurology as a junior resident.
 During the three days of the conference, I was in sessions revolving around different interesting topics in the field. I am highly interested in inflammatory diseases, and thanks to this opportunity I was able to attend multiple sclerosis discussions. The highlight of my journey was the plenary symposium about improving lives and reducing burden. It was interesting to me as a medical doctor from a low-income country.
During the three days of the conference, I was in sessions revolving around different interesting topics in the field. I am highly interested in inflammatory diseases, and thanks to this opportunity I was able to attend multiple sclerosis discussions. The highlight of my journey was the plenary symposium about improving lives and reducing burden. It was interesting to me as a medical doctor from a low-income country.
Overall, it was an enriching experience during which I had the opportunity to meet and connect with professors and residents in neurology from all over the world. We had various talks about our countries’ health systems, our current work, and future projects. I also had the honor to meet Dr. Claudio Bassetti.
Finally, I hope that I will have the opportunity to attend a conference again in the upcoming years to do presentations about the work that we do in my country. I hope these opportunities of travel fellowships will be more accessible for junior doctors/residents from low-income countries. •
Dr. Ben Mammou is a neurology resident in Tunis, Tunisia.
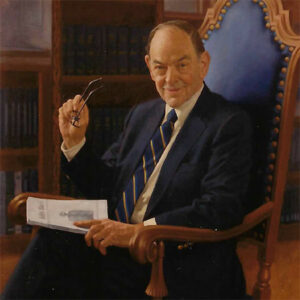 When Arthur K. Asbury, Van Meter professor of neurology emeritus at the Perelman School of Medicine of the University of Pennsylvania, died on Oct. 19, 2022, at the age of 93, the neurologic world lost a true giant, and many of us lost a friend and mentor.
When Arthur K. Asbury, Van Meter professor of neurology emeritus at the Perelman School of Medicine of the University of Pennsylvania, died on Oct. 19, 2022, at the age of 93, the neurologic world lost a true giant, and many of us lost a friend and mentor.

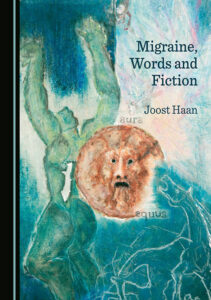 There is no objective test for migraine. Migraine cannot be proven with a scan, blood test, or EEG. The neurological examination during and outside attacks is usually normal. A diagnosis of “migraine” can only be made on the words with which patients describe past experiences. Their words must be “read” to get a diagnosis. Based on sparse, remembered, and metaphorical information, doctors worldwide make a diagnosis of migraine to distinguish it from, for example, tension-type headaches, a diagnosis that is also based on words.
There is no objective test for migraine. Migraine cannot be proven with a scan, blood test, or EEG. The neurological examination during and outside attacks is usually normal. A diagnosis of “migraine” can only be made on the words with which patients describe past experiences. Their words must be “read” to get a diagnosis. Based on sparse, remembered, and metaphorical information, doctors worldwide make a diagnosis of migraine to distinguish it from, for example, tension-type headaches, a diagnosis that is also based on words.

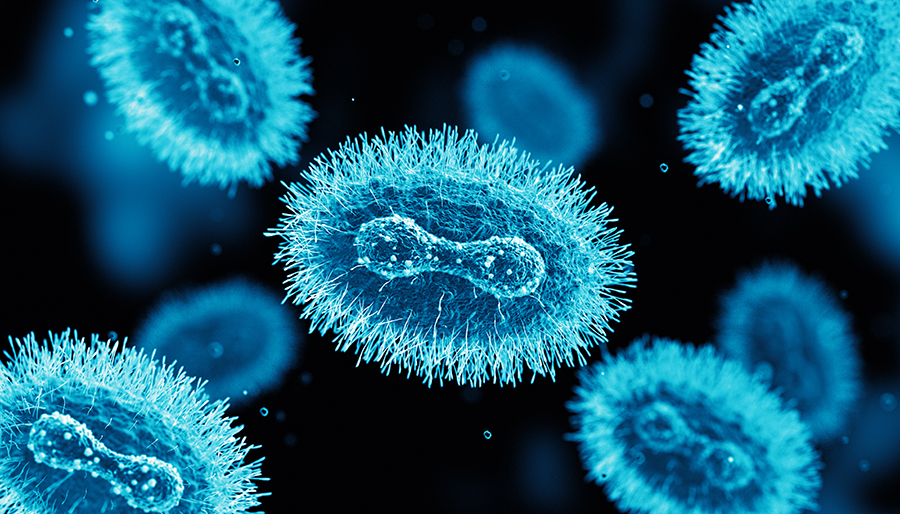 Neurological manifestations in the form of headache and malaise are observed in more than 50% of patients, while more serious complications like encephalitis and seizures are seen in less than 3% of patients.6 Anxiety and depression are common in hospitalized patients. Two cases of encephalitis due to monkeypox, both in girls requiring intubation and mechanical ventilation, are reported in the literature during past outbreaks7.
Neurological manifestations in the form of headache and malaise are observed in more than 50% of patients, while more serious complications like encephalitis and seizures are seen in less than 3% of patients.6 Anxiety and depression are common in hospitalized patients. Two cases of encephalitis due to monkeypox, both in girls requiring intubation and mechanical ventilation, are reported in the literature during past outbreaks7.
 The WFN’s policies regarding industry sponsorship, continuing medical education (CME), and conflicts of interest (COI) are provided here.
The WFN’s policies regarding industry sponsorship, continuing medical education (CME), and conflicts of interest (COI) are provided here. World Brain Day 2022 was celebrated with great fanfare and enthusiasm in India, and the campaign was extended over a week. This year’s theme “Brain Health for All” was appropriate, and it generated a lot of interest. Although the Dynamic President of the Indian Academy of Neurology (IAN) Nirmal Surya had given an ambitious target of 100 activities during the week, we ended up doing many more events across the country. The activities were focused on increasing awareness of common people and students about brain health and neurological diseases.
World Brain Day 2022 was celebrated with great fanfare and enthusiasm in India, and the campaign was extended over a week. This year’s theme “Brain Health for All” was appropriate, and it generated a lot of interest. Although the Dynamic President of the Indian Academy of Neurology (IAN) Nirmal Surya had given an ambitious target of 100 activities during the week, we ended up doing many more events across the country. The activities were focused on increasing awareness of common people and students about brain health and neurological diseases. Man Monahan Mehndiratta, chair, and Abhishek Shrivastava, convener of Neurorehabilitation subsection of IAN, conducted four webinars: Brain Health, Neuroplasticity—Rewiring the Brain, Cognition and Brain Health, and Update on Neuromodulation.
Man Monahan Mehndiratta, chair, and Abhishek Shrivastava, convener of Neurorehabilitation subsection of IAN, conducted four webinars: Brain Health, Neuroplasticity—Rewiring the Brain, Cognition and Brain Health, and Update on Neuromodulation.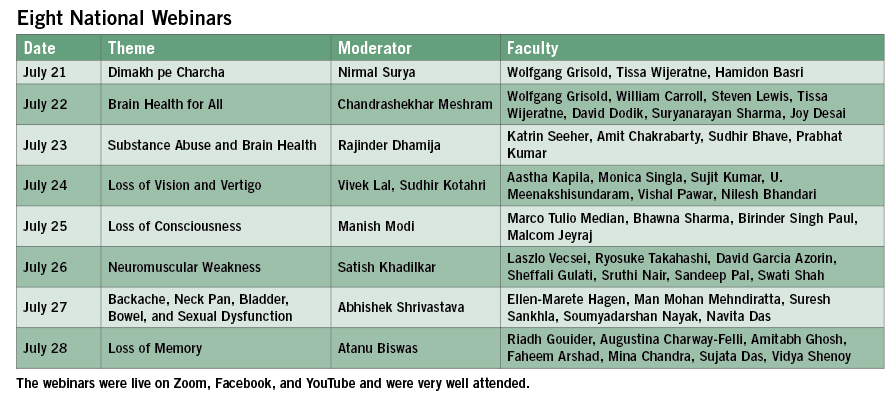 Nagpur—14 Activities Plus 43 Publications
Nagpur—14 Activities Plus 43 Publications  Suvarna Alladi and NIMHANs team organized a cricket match with cricketer Robin Uthappa who is brand ambassador of Karnataka’s brain health initiative. Policymakers, patients, care givers, institutional heads, and neurologists participated in the event. Karnataka Health Minister K. Sudhakar inaugurated the first of its kind brain health clinic in the Bangalore Hospital. It was supported by six newspaper publications. Amit Kulkarni delivered a public talk at Global Institute of Technology. Suryanarayan Sharma gave lectures in two colleges, and also at Toyota Industries. He organized the painting competition for school children. His interview was published in the newspaper and he did two digital platform activities. B. K. Madhusudan gave a talk at the university and had one Facebook live event on brain health.
Suvarna Alladi and NIMHANs team organized a cricket match with cricketer Robin Uthappa who is brand ambassador of Karnataka’s brain health initiative. Policymakers, patients, care givers, institutional heads, and neurologists participated in the event. Karnataka Health Minister K. Sudhakar inaugurated the first of its kind brain health clinic in the Bangalore Hospital. It was supported by six newspaper publications. Amit Kulkarni delivered a public talk at Global Institute of Technology. Suryanarayan Sharma gave lectures in two colleges, and also at Toyota Industries. He organized the painting competition for school children. His interview was published in the newspaper and he did two digital platform activities. B. K. Madhusudan gave a talk at the university and had one Facebook live event on brain health.