By Prof. William Carroll, WFN President

William Carroll, MD
Against the backdrop of what is without a doubt medical history – the vaccination of the world against SARS-Cov-2 virus (COVID-19) – it is appropriate to review our performance. That the vaccination rollout is bumpy is to be expected. That the world has developed a multitude of vaccines and that the process is under way in just over a year is outstanding.
What about the WFN? This assessment of the WFN is focused on the component parts of our organization rather than by overall achievement. In so doing, I hope to illustrate the effort and output of each.
- Member Societies
- Regional Organizations
- Individuals
- Related Organizations
- London Office
- Trustees
It is my personal perspective, and any errors or omissions are mine.
Member Societies
The member societies are the neurological bodies representing neurologists in each jurisdiction and are the core of the WFN. All have had to deal with the impact of the pandemic on their organization, function, and educational activities. In most instances, they have been successful. Members have continued to serve and care for neurological disorders, be involved in educational activities and training, and in many cases supported the World Brain Day campaign of 2020 and the first electronic Annual General Meeting of the Council of Delegates. Collectively, these efforts have assisted the WFN’s mission to foster brain health and quality neurology worldwide.
Member societies are the neurological bodies representing neurologists in each jurisdiction and are the core of the WFN.
117 of 122 member societies responded to the Needs Registry.
In addition, member societies have participated in the program to update communicability with the London Office, an essential element for our global organization. During this program, they have engaged in Zoom conversations to communicate their views on WFN activities and how they might be further engaged.
A pleasing 117 societies responded to the Needs Registry, which will provide data for the development of targeted campaigns to improve services and resources in all socioeconomic strata. Member societies in Africa and Mexico have, where possible, maintained WFN Training Programs.
Some member societies have seized the opportunity presented by the pandemic to upgrade their electronic educational program. Especially notable has been the efforts of the Indian Academy of Neurology in its highly regarded neuroinfections series of 2020, where it partnered with the Tropical and Geographical Neurology Specialty Group.
More recently, the IAN has begun a series highlighting the contribution made by inspiring leaders in neurology. (Please see WFN website.)
Regional Organizations
These six organizations through their presidents have attended the biennial WFN Strategy Meeting in 2020 at the time of the onset of the pandemic. Most of the six have continued their regular congresses.
Most of the six regional organizations have continued their regular congresses.
The EAN and AAN held successful virtual congresses in 2020 and plan to do so again in 2021. Both have also maintained close organizational ties through regular leadership meetings with the WFN.
The AOAN had to defer its 17th Congress from August 2020. It held a successful, highly regarded meeting in early April 2021, which was the first regional hybrid meeting. AFAN has deferred its scheduled biennial meeting from 2021 to October 2022 to be held in Cameroon.
With the WFN, AFAN held a valuable e-Learning Day on stroke in 2020, which included two parallel sessions in French. A similar e-Learning Day will be held in November 2021 on epilepsy.
PAUNS held its biennial Congress in February 2020 (at the onset of the pandemic) and will do the same in 2022.
PAFNS held its Congress in conjunction with the Brazilian Academy of Neurology in 2019 and plans its next congress for 2023.
Regional organizations are supporting efforts by a subgroup of trustees and office staff to improve communications.
Individuals
Neurologists are the core of each member society and the advocates and supporters for them and the WFN. They continue to participate in all regular activities of diagnosis, treatment, and care. In a number of instances, neurologists and neurological infrastructure have been drafted to COVID duties.
Many individuals have made, and are continuing to make, important contributions to national, regional, global, and disease-specific COVID-19 data collection efforts on topics ranging from the impact of COVID-19 on the provision of neurological services generally, the documentation of neuro-COVID phenotypes, and contributed to the development of the WHO Case Report Form to provide more uniform data collection. Many have also participated in activities overseen by the WHO Neuro-COVID Global Forum, the COVID-19 Neuroresearch Coalition, the EAN ENERGY Registry, the NINDS NeuroCOVID project, and the WFN Environmental Neurology Specialty Group’s list of registries.
Many neurologists continue to make important contributions to COVID-19 data collection and maintain neurological services.
Related Organizations
Members of the Global Neurology Alliance (GNA) have supported the WFN World Brain Day campaigns, especially the International Parkinson’s Disease and Movement Disorder Society (2020) and the Multiple Sclerosis International Federation (2021). Recently, GNA members have played a major role in the constructive assessment and advice to the WHO on its discussion plan for the preparation of the Intersectoral Global Action Plan for Epilepsy and Neurological Disorders. Notable here were the International League Against Epilepsy (ILAE,) International Bureau for Epilepsy (IBE), International Child Neurology Association (ICNA), World Stroke Organization (WSO), International Headache Society (IHS), the International Parkinson’s Disease and Movement Disorder Society (IPD&MDS), Alzheimer’s Disease International (ADI), the World Federation of Neuro-Rehabilitation (WFNR), World Psychiatry Association (WPA), and Multiple Sclerosis International Federation (MSIF).
A number of WFN Specialty Groups have also made valuable contributions to the WFN goals. I have already mentioned the Tropical and Geographical Neurology Specialty Group’s series on neuroinfections where they partnered with the Indian Academy of Neurology. The Migrant Neurology Specialty Group has produced an excellent comprehensive reference book on “Neurology for Migrants.”
The Rare Neurological Diseases Specialty Group is conducting a survey on these and their resourcing around the world. The new ALS/MND Diagnostic Criteria were published by the ALS/MND Specialty Group, and the Neuromuscular Disease Specialty Group held its 2020 Congress virtually.
London Office
If member societies are the core of the WFN, the London office is the heart. The WFN employed a second senior manager, Kimberly Karlshoej, in February 2020 with the primary role of overseeing new WFN initiatives, such as the Needs Registry and enhancing the relationship between the WFN and the WHO.
Within weeks, she joined the other London staff in lockdown. Despite the tribulations of the pandemic on London residents, the office staff have exceeded everyone’s expectations, including their own. They have maintained the routine day-to-day management of the federation, such as receiving and responding to email from member societies, calendar organization, financial, and membership records.
Where necessary, they have joined conference calls and provided audio recording for the production of accurate minutes despite an array of different time zones through countless Zoom, GoTo, Teams, and Webex meetings.
They guided a flawless Council of Delegates Annual General Meeting, including the inaugural electronic trustee election. They have orchestrated improved electronic communicability with member societies, specialty groups, WFN committees, and the Global Neurology Alliance, increased the social media posts, and assisted the regular website updates, including the COVID-19 and World Neurology page. These tasks, and there are many that I may have omitted, have all been performed with a cheerful professional disposition which has facilitated business operations in this unprecedented environment. I am sure I speak for all the trustees when I say that we are indebted to our office.
The London Office guided a flawless 2020 Council of Delegates Annual General Meeting, including the inaugural electronic trustee election.
The most important initiative they have been engaged in is the updating of member society contacts and the development of its enduring continuity.
Trustees
The pandemic began one month after the 2020 Trustees and Regional Presidents’ Strategy Meeting. At this time, Jean Marc Leger stepped down as co-opted trustee, and his place was taken soon after by Marianne de Visser. Both Leger and de Visser added invaluable depth to trustee discussions and decisions.
The expiration of Riadh Gouider’s stellar term as trustee at the 2020 AGM was also marked by the election of Morris Freedman. Freedman has begun to develop a WFN e-learning pilot program. Gouider continues to oversee the WFN/AFAN e-learning Day. Throughout 2020 and to date, each and every one of the trustees have combined energetically in the collective effort of the WFN. All have recognized the importance that they represent all member societies, and that decisions made by them, as trustees, are all gauged by their worth for the whole federation.
Trustees all recognize that they represent all member societies and that decisions made by them are gauged by their worth for the whole federation
It has been a pleasure to witness the careful consideration given by all in discussing a matter of weight before arriving at the most optimal decision. I have no doubt that the present composition of four officers, three elected trustees, and two co-opted trustees is the most efficient for a number of reasons.
First, a nine-person group is simply workable. Each can contribute readily both in discussion and in the preparation of papers for specific proposals. Second, the ability to co-opt two trustees provides flexibility for particular skillsets and diversity. Third, the staggered rotation of the elected trustees provides additional corporate memory to that of the executive officers. Fourth, a board of nine persons is a number that the London office can support efficiently. An increased number would likely require an increase in staff. Leanness and flexibility are two desirable virtues on which the WFN depends.
Current trustee structure is fit for purpose.
- A nine-person group is simply workable. Each can contribute readily both in discussion and in the preparation of papers for specific proposals.
- The ability to co-opt two trustees provides flexibility for particular skillsets and diversity.
- The staggered rotation of the elected trustees provides additional corporate memory to that of the executive officers.
- A board of nine persons is a number that the London office can support efficiently.
Conclusion
I am then unashamedly proud of the WFN and its robust advancement on all fronts despite the COVID-19 pandemic. As I have tried to illustrate above, every part of the organization, its governance, and the processes have performed admirably. I, as the president, and we all as the WFN, know that from individual neurologists, who have continued to function as neurologists in the care of people with neurological illness, through to the London office should share a sense of achievement for what has been done.
There is still some way to go to a post-COVID normal but we can appreciate that we will continue to prosecute our mission to foster brain health and quality neurology through and beyond the end of this pandemic. •


 We are also soliciting nominations of the names for WFN medals for 2021 ( https://wfneurology.org/activities/education-grants-and-awards/wfn-awards ).
We are also soliciting nominations of the names for WFN medals for 2021 ( https://wfneurology.org/activities/education-grants-and-awards/wfn-awards ).








 Let us spread the key messages from WBD 2021: Stop Multiple Sclerosis through mainstream media, social media platforms, and local, regional, national and international meetings throughout the year. Please see and share our new logo, the web banners, social media images, and other educational material in your country. We invite our readers to rally around WBD 2021 with the aim to stop multiple sclerosis.
Let us spread the key messages from WBD 2021: Stop Multiple Sclerosis through mainstream media, social media platforms, and local, regional, national and international meetings throughout the year. Please see and share our new logo, the web banners, social media images, and other educational material in your country. We invite our readers to rally around WBD 2021 with the aim to stop multiple sclerosis.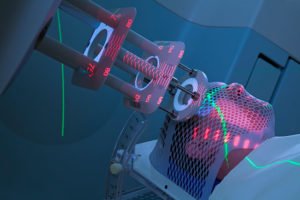 Cancer is one of the most important conditions in human health, and due to longer life expectation and improved therapies, survival in cancer patients is also increasing. This has several implications in the management of cancer patients as the longer survival changes the “natural” course of many tumors.
Cancer is one of the most important conditions in human health, and due to longer life expectation and improved therapies, survival in cancer patients is also increasing. This has several implications in the management of cancer patients as the longer survival changes the “natural” course of many tumors.




