Hany Naref and Nevine El Nahas

Hany Naref, Nevine El Nahas
On the afternoon of June 30, 2014, while she was preparing food for her family in a fasting day of Ramadan, she suddenly felt weakness in her left arm, with speech difficulty, and she asked her daughters for help. Two hours later, she presented to our stroke unit.
Knowing the importance of acting rapidly, the resident immediately ordered a CT scan brain and laboratory workup. Then the resident discussed the feasibility of thrombolysis. However, the responses of the radiology and laboratory staff were rather slow, as they did not appreciate the urgency of the situation.
The brain CT eventually showed that she was eligible for thrombolysis; however, we were left with one and a half hours for the window to close. Moreover, rtPA was not available in our hospital. Also, we had to pay for it. The senior staff (having donations from the department staff) decided to buy it from the nearest pharmacy. Several pharmacies were contacted until it was finally sourced and dispatched just 15 minutes before the end of the window.
The patient started to move her limbs one hour after receiving rtPA.
“Ma’am, what were you been doing when you got this stroke?” our resident asked.
In an intelligible speech, she said:
“I was cooking chicken and soup for my children to eat after a long fasting day. I thought I would never be able to cook for my kids anymore.”
With a smile of satisfaction, our resident said:
“Well, Happy Ramadan. Now you have recovered from the stroke, and you will go back and cook for your children.”

Certificate of accreditation of Ain Shams University stroke centers.
In 2014, rtPA was used in less than 1% of stroke cases and was not reimbursed by the Egyptian Ministry of Health (MOH). This case was a spark that ignited a sequence of corrective actions for acute stroke management. The stroke team at Ain Shams University (ASU) conducted research to identify the obstacles for reperfusion therapy, and by the end of 2015, an action plan was instituted. Neurology residents and nursing staff received training, and a guidelines manual for reperfusion therapy was established. Concomitantly, fundraising started in the ASU stroke unit to provide rtPA through donations. In a 6-month period, the rate of thrombolysis increased significantly to reach 12.3% of all cases of ischemic strokes1.
As a result of this advocacy, the MOH was convinced to reimburse rtPA, and all the Egyptian universities were tempted to pursue the same track as ASU. The number of stroke units increased from 20 to reach 95 by 2020. Then, in collaboration with the Ministry of Higher Education, university stroke units became hubs for satellite stroke-ready hospitals that are under the umbrella of MOH2.
Due to the progress in stroke services, in 2018, thrombectomy became reimbursed by MOH. Thus, the number of thrombectomies increased from 17 cases in 2016 to 172 in 2019.
In addition, by 2018, the first telestroke unit in Egypt was introduced in ASU. It started to provide consultation to neurologists for stroke management in remote hospitals2.
The rate of acute stroke therapy kept steadily developing with a reduction of door-to-needle time and improvement of patient outcomes. This ultimately led to accreditation of the two stroke units of ASU by the German Stroke Society in August 2019 in addition to receiving ESO and WSO Angels awards3.
We started our journey by searching for rtPA in nearby private pharmacies, and now all types of reperfusion therapies are available and reimbursable, with door-to-needle time less than 1 hour4. Currently, we are expecting the launch of our new stroke unit with an angio-suite installed inside the unit to achieve door-to-angio service. It also comprises an acute rehabilitation facility, gait lab, and a dedicated neurosonology unit. The stroke patient journey in Cairo now is smooth with a much-improved outcome than it was 10 years ago. •
Hany Naref is professor of neurology at Ain Shams University, and Nevine El Nahas is professor of neurology and head of the stroke unit and neuromodulation lab at Ain Shams University.
References:
-
Zakaria MF, Aref H, Abd ElNasser A, Fahmy N, Tork MA, Fouad MM, et al. Egyptian experience in increasing utilization of reperfusion therapies in acute ischemic stroke. Int J Stroke. 2018; 13(5): 525–9.
-
Hacke W, Caso V, Esagunde RU, Aref HM, Martina S, Mikulik R. Stroke care taking flight with the wings of ANGELS. A symposium presented by Boehringer Ingelheim at the ESO-WSO Virtual Conference 2020 Nov 8. 2021; 6: 8–25.
-
“ESO and WSO”. Available from: https: //www.angels-initiative.com/angels-awards.
-
El Nahas NM, Shokri HM, Roushdy TM, Dawood NL, Abushady EM, Georgy SS, Zaki AS, Bedros RY, Aref HM. Door to Needle Count Down: A 3-Years Experience in an Egyptian University Stroke Center. Neurologist. 2021 Nov 30;27(2):61-64. doi: 10.1097/NRL.0000000000000372. PMID: 34855665.

 This year’s meeting on environmental health took place over two days and in a hybrid format in order to allow active participation unencumbered by travel. Participants and speakers from all over the world were able to gather, report findings as well as discuss relevant topics. Day 1 included sessions on neurotoxicology, exposure science, and the clinical approach of exposure sciences. Day 2 included neurological impacts of climate change, health impacts of air pollution, long COVID as well as diseases and environmental risk factors.
This year’s meeting on environmental health took place over two days and in a hybrid format in order to allow active participation unencumbered by travel. Participants and speakers from all over the world were able to gather, report findings as well as discuss relevant topics. Day 1 included sessions on neurotoxicology, exposure science, and the clinical approach of exposure sciences. Day 2 included neurological impacts of climate change, health impacts of air pollution, long COVID as well as diseases and environmental risk factors. The 17th International Summer School of Neurology took place July 8-10, 2022, and was organized as a hybrid event. This educational activity along with the Fifth Teaching Course on Rare Neurological Diseases, brought together a lively audience of over 1,400 participants in a hybrid format, both online and on-site. In addition, the 3-day event hosted an online parallel session, “Psychiatry Perspectives in Neurocognitive Disorders” and a satellite session (on-site, on the shores of the Black Sea in Romania), focused on clinical case studies. This session was coordinated by Prof. Raad Shakir (UK), CBE, former World Federation of Neurology (WFN) president. The event was organized by Prof. Dafin Muresanu (Romania) and presided over by well-established international specialists, such as WFN President Wolfgang Grisold (Austria), Natan Bornstein (Israel), Volker Homberg (Germany), and Raad Shakir (UK). In addition, the events featured strong collaboration and endorsement from the World Federation of Neurology (WFN), the World Federation of Neurorehabilitation (WFNR), the European Federation of Neurorehabilitation Societies (EFNR), and the European Academy of Neurology (EAN), among other institutions.
The 17th International Summer School of Neurology took place July 8-10, 2022, and was organized as a hybrid event. This educational activity along with the Fifth Teaching Course on Rare Neurological Diseases, brought together a lively audience of over 1,400 participants in a hybrid format, both online and on-site. In addition, the 3-day event hosted an online parallel session, “Psychiatry Perspectives in Neurocognitive Disorders” and a satellite session (on-site, on the shores of the Black Sea in Romania), focused on clinical case studies. This session was coordinated by Prof. Raad Shakir (UK), CBE, former World Federation of Neurology (WFN) president. The event was organized by Prof. Dafin Muresanu (Romania) and presided over by well-established international specialists, such as WFN President Wolfgang Grisold (Austria), Natan Bornstein (Israel), Volker Homberg (Germany), and Raad Shakir (UK). In addition, the events featured strong collaboration and endorsement from the World Federation of Neurology (WFN), the World Federation of Neurorehabilitation (WFNR), the European Federation of Neurorehabilitation Societies (EFNR), and the European Academy of Neurology (EAN), among other institutions. Thanks to World Federation of Neurology, I had the opportunity to attend the Eighth European Academy of Neurology Congress June 25-28, 2022, in Vienna Austria.
Thanks to World Federation of Neurology, I had the opportunity to attend the Eighth European Academy of Neurology Congress June 25-28, 2022, in Vienna Austria. During the three days of the conference, I was in sessions revolving around different interesting topics in the field. I am highly interested in inflammatory diseases, and thanks to this opportunity I was able to attend multiple sclerosis discussions. The highlight of my journey was the plenary symposium about improving lives and reducing burden. It was interesting to me as a medical doctor from a low-income country.
During the three days of the conference, I was in sessions revolving around different interesting topics in the field. I am highly interested in inflammatory diseases, and thanks to this opportunity I was able to attend multiple sclerosis discussions. The highlight of my journey was the plenary symposium about improving lives and reducing burden. It was interesting to me as a medical doctor from a low-income country. When Arthur K. Asbury, Van Meter professor of neurology emeritus at the Perelman School of Medicine of the University of Pennsylvania, died on Oct. 19, 2022, at the age of 93, the neurologic world lost a true giant, and many of us lost a friend and mentor.
When Arthur K. Asbury, Van Meter professor of neurology emeritus at the Perelman School of Medicine of the University of Pennsylvania, died on Oct. 19, 2022, at the age of 93, the neurologic world lost a true giant, and many of us lost a friend and mentor.

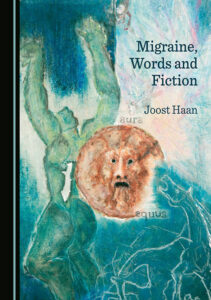 There is no objective test for migraine. Migraine cannot be proven with a scan, blood test, or EEG. The neurological examination during and outside attacks is usually normal. A diagnosis of “migraine” can only be made on the words with which patients describe past experiences. Their words must be “read” to get a diagnosis. Based on sparse, remembered, and metaphorical information, doctors worldwide make a diagnosis of migraine to distinguish it from, for example, tension-type headaches, a diagnosis that is also based on words.
There is no objective test for migraine. Migraine cannot be proven with a scan, blood test, or EEG. The neurological examination during and outside attacks is usually normal. A diagnosis of “migraine” can only be made on the words with which patients describe past experiences. Their words must be “read” to get a diagnosis. Based on sparse, remembered, and metaphorical information, doctors worldwide make a diagnosis of migraine to distinguish it from, for example, tension-type headaches, a diagnosis that is also based on words.
