Resolution WHA 73.10 for the Development of an Intersectoral Global Action Plan (IGAP) on Epilepsy and Other Neurological Disorders. 2022 – 2031.
By Kimberly Karlshoej on behalf of Alla Guekht, Wolfgang Grisold, Sam Wiebe, Helen Cross, Julie Hall, Martin Brodie, Mary Secco, Jo Wilmhurst, Michael Brainin, Claudia Trenkwalder, David Dodick, and Bill Carroll

Kimberly Karlshoej
It was a landmark event when on Nov. 12, 2020, the WHO Executive Board accepted the recommendation of the World Health Assembly (WHA) to adopt Resolution WHA73.10. This resolution called for the development of an Intersectoral Global Action Plan (IGAP) to tackle epilepsy and other neurological disorders through comprehensive actions to detect, prevent, care, treat, and rehabilitate people with epilepsy and other neurological disorders, as well as ensuring their social, economic, educational, and inclusion needs.
The WFN has long been involved with neurological activities with the WHO, which include a first edition of the Atlas: Country Resources for Neurological Disorders 2004, Neurological Disorders: Public Health Challenges 2006 and the second edition of the Atlas: Country Resources for Neurological Disorders 2017, to mention a few. The resolution to develop an IGAP is also momentous in that neurological disorders are overtly recognized by the WHO Member States in line with the Global Burden of Neurological Disorders (2018) finding of them being the leading cause of disability-adjusted-life-years and the second leading cause of death.
The resolution is in large part due to the efforts of the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE) supported strongly by the WFN who, with several member states led by the Russian Ministry of Health, convinced the WHA that epilepsy was a public health emergency. In the lead up to Resolution WHA 73.10, member states recognized the burden of epilepsy and the synergies with many neurological conditions, especially access to both services and support for such conditions was insufficient, especially in low- and middle-income countries. The vote to address the problem with the call for the IGAP was unanimous. The WFN has a unique opportunity to contribute to the development of the IGAP.
As the first step, the WHO published a discussion paper. The WFN as a “non-state actor” (NSA) in official relations with WHO presented its comments on the draft discussion paper in both virtual and web-based consultations. To do this, the WFN first joined with the ILAE, IBE, and the International Child Neurology Association (ICNA) to formulate comments on epilepsy and other neurological disorders, both adult and children, to match the intent of the IGAP draft discussion paper.
Second, the WFN formed a separate group with members of the Global Neurology Alliance (GNA) to advocate a stronger voice for neurological conditions. This group was selected by WFN President William Carroll to reflect the conditions that contributed most to the Global Burden of Neurological Disorders. The group comprised immediate past presidents of the International Headache Society (IHS: David Dodick), World Stroke Organization (WSO: Michael Brainin) and the current President of the Parkinson’s Disease and Movement Disorders Society (MDS: Claudia Trenkwalder) together with Alla Guekht, Wolfgang Grisold, and Kimberly Karlshoej from the WFN. Alla Guekht was indispensable in these meetings through her knowledge of the WHO. The WFN contributions to the WHO discussion plan were made jointly with the ILAE, IBE, and ICNA and jointly with the WSO, MDS, and IHS.
As social, biological, and environmental determinants mediate all experience, including responses to stress, and impact on brain development and brain health from pre-conception to end-of-life, the WFN emphasized in its submission the need for countries to prioritize brain health in their policies. New strategies for both brain health promotion and disease prevention across the life course need to be implemented at national levels.
Addressing the costs of health care, and reducing the current treatments gaps, especially in low resource settings was also emphasized.
Finally, the WFN stressed the importance of addressing stigma, exclusion, and discrimination of people with neurological disorders in its submission.
These general comments as well as many specific ones on the discussion paper were submitted to the WHO April 10 and were published with the other submissions as consolidated comments by WHO. The WHO then developed the first draft of the Intersectoral global action plan on epilepsy and other neurological disorders (IGAP) based on the input received. This document outlines the scope, vision, goal, and strategic objectives as well as specific actions for Member States, the WHO Secretaria, and international and national partners.
Further consultation on this draft document began during July 2021, and the WFN worked with the same two groups: first, the ILAE and ICNA, and second, the WSO, IHS, and MDS. Central to these submissions was to make the first draft more evenly balanced in its intent. Instead of recommending epilepsy as the entry point for all interventions in the implementation of IGAP, essentially a hierarchical approach, the WFN joint submissions recommended that implementation be undertaken with prioritisation determined by member states as either epilepsy with neurological disorder(s), neurological disorder(s) alone, or epilepsy alone depending on the member states needs and abilities. The WFN and its partners remained fully supportive of the need for a specific global action plan for epilepsy within IGAP. The outcomes of these consultations will serve as input for the WHO Secretariat to prepare a revised draft of IGAP that will be submitted for review at the 150th session of the Executive Board in May 2022. •
Kimberly Karlshoej is strategy and program director for the WFN.


![George Kenneth York III]](https://worldneurologyonline.com/wp-content/uploads/2021/09/York_web-150x200.jpg)

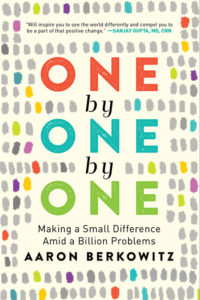 Over this past year, we have all come to wonder what we can do to make a difference in the face of problems that seem so overwhelming. When we think about the scope of the pandemic and other global health issues, the devastating numbers are heart breaking, and it’s easy to lose sight of the individual people and stories behind the statistics. In Aaron Berkowitz’s new book, “One by One by One,” he shares with us the lessons he learned as he tried to make a small difference by helping one individual at a time amid suffering measured in billions.
Over this past year, we have all come to wonder what we can do to make a difference in the face of problems that seem so overwhelming. When we think about the scope of the pandemic and other global health issues, the devastating numbers are heart breaking, and it’s easy to lose sight of the individual people and stories behind the statistics. In Aaron Berkowitz’s new book, “One by One by One,” he shares with us the lessons he learned as he tried to make a small difference by helping one individual at a time amid suffering measured in billions.