WFN president reviews neurology development around the world, IGAP, World Brain Day, WCN, and other key topics.
Wolfgang Grisold
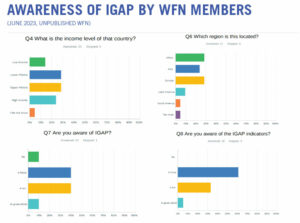
A 2023 WFN survey of WFN member societies assessing knowledge and content of the IGAP, revealed a disconcerting low level and awareness. Activities and publications of the WFN are aimed to increase the awareness and practical implementation of IGAP (Displayed Q 4-8) (London Office: C. Hunte)
Welcome to the first issue of World Neurology in 2024. We hope you had a relaxing, festive holiday season, and we look forward to the new year. 2024 will be another positive year for neurology, and we as the neurological community of the WFN will have many opportunities to foster and support neurology.
Globally, neurology is developing well. This statement can be supported by developments in neuroscience and global developments. General neurology as well as the subspecialties are thriving; examples are stroke and worldwide stroke services, epilepsy, and new drugs for epilepsy, movement disorders, and MS. The new possibilities not only to diagnose, but also to treat some of the genetic diseases is an incredible advance, and breaks previous dogmas on therapy limitations and prognosis of some neurological diseases.
Regarding global development, important are the activities of the WHO. Worldwide, the WHO has 194 member states. Several WHO departments take care of present and emerging health problems of the world. The classification of neurological disorders still needs separation from mental disorders and requires a universal and globally accepted classification, which can be the basis for universally applied stable and more devoted structures.
A positive example for the development of classification is stroke and ICD-11, where the WHO ICD-11 classification will allow further implementation of stroke services worldwide. Despite this amazing success story, we must continue to develop the prevention as well as chronic care, disability, and palliative care in stroke patients on the other side of the spectrum.
The WHO has implemented a “brain health unit” that fosters and supports the implementation and development of neurology. One key development is the IGAP, which is based on policy and advocacy, therapy, prevention, innovation, research, and public health. This concept was accepted by all member states at the World Health Assembly in 2022. Despite its strong support for neurology and ultimately persons with neurological diseases, the echo and acceptance at the regional and country level still needs more powerful inputs.
Presently, the WHO is developing a tool kit for the implementation of IGAP, addressing all stakeholders. The WFN uses its channels of distribution to member societies, uses information at talks and presentations, has information on IGAP on its website, and has emphasized the IGAP and cooperation with the WHO at the World Congress of Neurology (WCN) 2023 and will continue to do so.
We want to emphasize this important IGAP activity for several reasons:
- It promotes neurology at all levels and everywhere (“Semper et unique“).
- It provides a well-structured concept on the establishment and needs of neurology, which can be adapted and used according to the individual local needs. This may differ according to the income status of countries.
The call to all member societies is to familiarize members and health systems with the IGAP, put it on the agenda of your society meetings, and try to promote it within your networks, including health authorities and other stakeholders.
The mission of IGAP and the role for the development of neurology is enormous. We want to remind readers of the important role of the ILAE and the WFN in its development. We share this common effort, and as stakeholders, we have to avoid competitive altruism. The common goal is implementation of neurology and improvement of the large number of persons affected with acute and chronicneurologic disorders, disability, and be on the forefront to prevent disease.
From the other tasks and programs of the WHO, such as brain health, fight meningitis and tuberculosis, and implementation of rehabilitation, we would like to remind readers of the WHO essential medicine list (EML), which we covered in the last issue of World Neurology in 2023. Successfully, more medications, one for epilepsy and two for MS, were added to the EML list. The EML is a dedicated WHO effort to make drugs available in all countries of the world. In some countries, there is a lack of registered drugs, deficits in registration, procurement, distribution, and affordability.
World Brain Day (WBD)
The WBD has become an annual event for the WFN community. It celebrates the day of WFN’s founding in 1957, chooses a yearly topic, and collaborates with topic-related societies and regions.
This year, we will continue supporting the important topic of brain health, and focus on brain health and prevention. The activities will be chaired by D. Dodick and T. Wijeratne, the WFN regions, and will receive professional help from the marketing firm Yakkety Yak.
Prevention in neurology is a powerful and often underestimated tool to prevent neurological diseases and has a wide range of interventions, from vaccination, to pharmacology, nutrition, and lifestyle modifications. As with diagnosis and treatment, all types of prevention need to be added to neurological curricula.
Communication: Meetings/Congresses and Education
Communication with the WFN‘s member societies is important. Please follow our website and social media. We also have a new medium called the WFN Service Page, which will be published every three months in the Journal of the Neurological Sciences (JNS). This will increase the reach of the WFN. We also encourage you to publish material from your society and your regions in World Neurology. If you consider publishing in a journal, please consider the JNS and eNS as official journals of the WFN.
Congresses such as the WCN 2023 always leave impressions and produce new insights, either at the meeting or in discussions and informal gatherings. We are happy to report we had a large number of persons participating virtually at this congress. This served two main purposes: to reach countries worldwide, who are unable to travel for financial and other reasons, and to increase the worldwide spread of neurology. One hundred and thirty two countries participated.
There is material on the WFN website from the WCN 2023 in Montreal. Also, please note the summary of the plenary sessions, the coffee talks, and all abstracts are now published in the JNS.

Meeting with the Korean Committee in Seoul.
The next WCN will be in Seoul in 2025. The program committee has started its work. It is a generous venue and and a vibrant city. The Korean Neurological Society is putting much effort into this important congress, and it will provide strong input for neurology in the region.
For September 2024, we are planning a virtual educational update meeting: World Federation of Neurology Digital Update 2024 (WNU2024) Sept. 26-27. Eminent speakers will provide an update on the most frequent diseases, and the meeting will offer online teaching courses on these topics.
It will be a useful update instrument between the WCN congresses. Updates, education, and CME will be the strategy. The meeting will be virtual only.
WFN educational days will be continued, with the AFAN WFN educational day on neuropathies on Feb. 17, 2024, followed by a joint headache day with AFAN and GPAC/IHS. Another educational day with the AOAN is planned. This format has been successful, attracting many attendees, not only from the regions, but worldwide. Recordings of the meeting can be seen in the WFN e-learning hub.

The WFN president high above Seoul.
We need to encourage and increase our efforts for CME and continuous professional development (CPD) worldwide. This is an essential part of professional practice in neurology, and needs constant update and development. Worldwide, many countries have established CME programs, belonging to the portfolio of practicing neurologists and are often linked with recertification. Usually the time of participation in a meeting or an activity is converted into a system of credits. This works well for individual countries but, for many reasons, in most circumstances cannot be exchanged or compared.
For large international congresses such as the WCN, the UEMS EACCME system is used, which has a detailed and strict separation of industry and other possible influences on the scientific program. This system is acknowledged by most European countries, and it also has an agreement with the American Medical Association and the Canadian Royal College of Physicians.
The WFN has a Standards and Evaluation Committee (chaired by Prof. Laszlo Vescey) in place that receives applications for meetings and events which fulfil the criteria of the WFN . This committee endorses international meetings according to the requirements of the WFN. The endorsed meeting is allowed to use the WFN logo for its event.
This was a short update on important WFN activities. Please follow us on our website and social media as well as the new WFN service page in JNS for more information. •
 By Wolfgang Grisold
By Wolfgang Grisold
 By Prisca-Rolande Bassolé, MD
By Prisca-Rolande Bassolé, MD Hosted in Montreal, the 2023 World Congress of Neurology united experts to address key neurology challenges. Plenary speakers shared their latest research on topics such as diabetic neuropathies, Parkinson’s disease, ALS, and global health care equity.
Hosted in Montreal, the 2023 World Congress of Neurology united experts to address key neurology challenges. Plenary speakers shared their latest research on topics such as diabetic neuropathies, Parkinson’s disease, ALS, and global health care equity.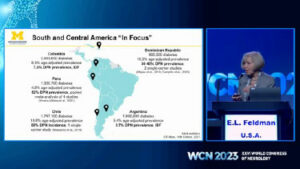

 By Chandrashekhar Meshram
By Chandrashekhar Meshram Jan van Gijn hardly needs an introduction. He is well known for his clinical research of cerebrovascular disorders. He chaired the Utrecht team that made many contributions to our knowledge of different types of stroke, notably transient ischemic attacks and aneurysmal subarachnoid hemorrhage. Many participants of stroke conferences will remember his well-designed presentations, often illustrated with paintings by Dutch masters.
Jan van Gijn hardly needs an introduction. He is well known for his clinical research of cerebrovascular disorders. He chaired the Utrecht team that made many contributions to our knowledge of different types of stroke, notably transient ischemic attacks and aneurysmal subarachnoid hemorrhage. Many participants of stroke conferences will remember his well-designed presentations, often illustrated with paintings by Dutch masters. In the foreword, the author mentions some pitfalls for amateurs who write about the history of their own profession. One is consulting secondary, translated, and often unreliable sources. A second is known as presentism, the fallacy to reconstruct history, looking back from the vantage point of today’s knowledge, as a rational process that leads in a straight line, through a sequence of major discoveries to the present. Van Gijn has avoided these pitfalls by thorough preparation. He studied Latin and enrolled as a student of history and philosophy of science.
In the foreword, the author mentions some pitfalls for amateurs who write about the history of their own profession. One is consulting secondary, translated, and often unreliable sources. A second is known as presentism, the fallacy to reconstruct history, looking back from the vantage point of today’s knowledge, as a rational process that leads in a straight line, through a sequence of major discoveries to the present. Van Gijn has avoided these pitfalls by thorough preparation. He studied Latin and enrolled as a student of history and philosophy of science.



 One must first realize that more than three-quarters of the disease burden resides in regions that are struggling to bridge the treatment gap. In a world where everything is run by money, the catastrophic expenditure on health burdens every family in the lesser privileged sections of economy. This expenditure encompasses costs of medication, hospitalization, and continuation of care. The onus to balance livelihood and health falls on the patient, and when this burden becomes too much, they tend to stop being compliant to treatment — an ignition to the vicious cycle of expense and hospitalization.
One must first realize that more than three-quarters of the disease burden resides in regions that are struggling to bridge the treatment gap. In a world where everything is run by money, the catastrophic expenditure on health burdens every family in the lesser privileged sections of economy. This expenditure encompasses costs of medication, hospitalization, and continuation of care. The onus to balance livelihood and health falls on the patient, and when this burden becomes too much, they tend to stop being compliant to treatment — an ignition to the vicious cycle of expense and hospitalization.  Among the patient stories we have permission to share was of one college student on three anti-seizure medicines. He often received different injections in the emergency department and was prescribed different cocktails of medicines due to his lack of record keeping. But with this app, he is documenting his prescriptions and scans and has currently been seizure free for eight months. The most useful feature for him, “For me, the drug reminder alarm is a huge help, and it makes sure I have not missed medications like I used to before.”
Among the patient stories we have permission to share was of one college student on three anti-seizure medicines. He often received different injections in the emergency department and was prescribed different cocktails of medicines due to his lack of record keeping. But with this app, he is documenting his prescriptions and scans and has currently been seizure free for eight months. The most useful feature for him, “For me, the drug reminder alarm is a huge help, and it makes sure I have not missed medications like I used to before.” By Marco Tulio Medina, FAAN, FEAN
By Marco Tulio Medina, FAAN, FEAN In May 2022, the Assembly of the World Health Organization (WHO) approved the Global Intersectoral Action Plan (IGAP) for Epilepsy and other Neurological Disorders, so that between 2022 and 2031, the countries of the world can improve the approach to brain health through specific actions for prevention, treatment, rehabilitation, and palliative measures.
In May 2022, the Assembly of the World Health Organization (WHO) approved the Global Intersectoral Action Plan (IGAP) for Epilepsy and other Neurological Disorders, so that between 2022 and 2031, the countries of the world can improve the approach to brain health through specific actions for prevention, treatment, rehabilitation, and palliative measures. In Honduras, after a process of community intervention, we were able to reduce the frequency of a cerebral parasitosis, neurocysticercosis (incorrectly called “triquina” in Honduras), caused by fecal contamination by tapeworm or Taenia solium worms, in Salama, Olancho, through environmental sanitation measures and the educational campaign “the piggy is not to blame,” among others. Access to anti-epileptic drugs was also improved, thereby reducing the treatment gap.
In Honduras, after a process of community intervention, we were able to reduce the frequency of a cerebral parasitosis, neurocysticercosis (incorrectly called “triquina” in Honduras), caused by fecal contamination by tapeworm or Taenia solium worms, in Salama, Olancho, through environmental sanitation measures and the educational campaign “the piggy is not to blame,” among others. Access to anti-epileptic drugs was also improved, thereby reducing the treatment gap. The creation of this postgraduate program had many detractors, who argued that there were not the necessary conditions in Honduras for its development, but despite these critics, the postgraduate course was certified worldwide for its high quality in 2006 by the WFN and named a WHO collaborating center for research and community intervention in epilepsy (HON01), thus supporting the Strategic Plan and action of the Pan American Health Organization (PAHO) between 2011 and 2022.
The creation of this postgraduate program had many detractors, who argued that there were not the necessary conditions in Honduras for its development, but despite these critics, the postgraduate course was certified worldwide for its high quality in 2006 by the WFN and named a WHO collaborating center for research and community intervention in epilepsy (HON01), thus supporting the Strategic Plan and action of the Pan American Health Organization (PAHO) between 2011 and 2022.