By Ani-Osheku Ifeyinwa, Nigeria

Neurology Grand Rounds
In December 2019, I had the utmost privilege to spend four weeks at the neurology department of the Selçuk University in Konya, Turkey. It remains one of the most gratifying moments in my career as a young neurologist.
It has been over a year, yet the memories are ever so fresh. I clearly remember the feeling of excitement as I walked into the massive Selçuk University Hospital and made my way to the “nöroloji poliklinik” where I was greeted with so much warmth by the entire neurology staff. I met Prof. Şerefnur Öztürk, my supervisor, who provided me with the itinerary and a road map of what I was to expect in the coming weeks.
Indeed, it was a four-week period of intense learning in a relaxed and friendly environment. I had the privilege of exploring the world of the practice of neurology by the Turks under the able guidance and excellent mentorship of the neurology team of the Selçuk University Hospital.

Certificate presentation and the new year celebration.
Case after case, I witnessed the translational art of the pathological basis of neurologic diseases from therapeutic theorem to practical strategies using cut-edge technology and evidence-based medicine in the management of various neurologic conditions, including stroke, movement disorders, demyelinating disease (especially multiple sclerosis), neuromuscular diseases, and seizure disorders.
Prof. Öztürk shared with me priceless clinical pearls especially in the area of vascular neurology during the daily morning rounds in the neuro-intensive service as well as in the outpatient service. Her depth of knowledge combined with her wealth of experience has inspired me to push the limits of my career.
It was intriguing watching Prof. Gökhan Özdemir navigate stenosed and occluded vessels inserting stents and retrieving clots and ultimately achieving revascularization.
My experience with the neurophysiology laboratories left quite an impression on me that instinctively I knew I would pursue a fellowship in this area. I participated in carrying out and interpreting several EEGs, needle EMGs, and nerve conduction studies under the supervision of Profs. Gökhan Özdemir, Haluk Gümüş, and Dr. Hakan Ekmekci.
I learned the techniques of peripheral nerve blockade in the management of headaches and this service is one of the treatment modalities currently offered to patients with headache disorders in our neurology clinic. The ease of application coupled with the dramatic improvement has been a rewarding experience.

Lunch with neurology residents
I joined the neurosurgical team in the collaborative management of patients especially those with movement disorders, where I witnessed the usefulness of deep brain stimulation in advanced Parkinson’s disease.
One of the highlights of my stay was the opportunity to speak on “Nigeria, Its People, and Its Health Care System: A Focus on Neurological Diseases.” This lecture was delivered on Dec. 25, 2019, in the Dekanlik Donem 2 Amfisi, and I tagged it “A Christmas to Remember!”
The rich cultural heritage of the Turks makes the city a tourist’s delight. I savored the tastebud tantalizing Turkish foods and enjoyed the sceneries of some of the city’s famous sites, like the famous Mevlâna Museum and Alaaddin Cami.
Despite the numerous challenges the novel Covid-19 pandemic brought, redefining interactions in the health care sector along with restrictions in movements that put a hold on dreams for the physical quest in knowledge acquisition, I have continued to cascade the knowledge so acquired in my time in Selçuk in order to positively impact the lives of patients with neurological needs in Nigeria. I am currently working on various projects that include the transfer of skills acquired, especially relating to headache management and protocols for managing various neurology conditions.
Dr. Ani-Osheku Ifeyinwa giving a lecture
My profound gratitude to the WFN/TNS for this wonderful and innovative collaboration to give young neurologists like me the opportunity to experience the practice of neurology in an advanced society and a chance to improve our skills and broaden our horizons. Plenty of thanks to Mrs. Jade Levy and Mr. Burak for the seamless facilitation of my trip and stay in Konya. My deep appreciation to Selçuk University and the dean of the College of Medicine for providing the enabling environment for my visit. To Prof. Şerefnur Öztürk, you inspire me in numerous ways to be the best version of myself. Finally, to the exceptional team at the Selçuk neurology department that showed me true friendship, generosity, and ensured I was well integrated, I say thank you!
I had the most amazing time in Konya and established alliances that I believe will go a long way. The lessons learned from my four weeks to Selçuk University will always be a reference point in my career development. •
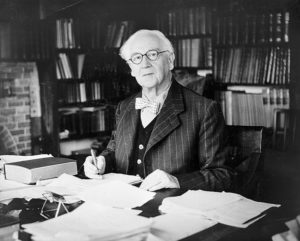
 Prof. Raad Shakir has been a prominent figure in neurology in the United Kingdom for more than 20 years and was one of the key persons in the organization of the successful London 2001 World Congress of Neurology. His contributions to both neurology in the U.K. and to the World Federation of Neurology (WFN) have been witnessed by many.
Prof. Raad Shakir has been a prominent figure in neurology in the United Kingdom for more than 20 years and was one of the key persons in the organization of the successful London 2001 World Congress of Neurology. His contributions to both neurology in the U.K. and to the World Federation of Neurology (WFN) have been witnessed by many.

 As the chair of the Congress Committee, I cordially invite you to join the 25th World Congress of Neurology (WCN) to be held Oct. 3-7, 2021, in Rome, Italy. Since the pandemic of COVID-19 will not completely fade out by then, we are most likely to have a hybrid-type congress, providing you the option of attending in person or virtually. The committee has decided that we will remain flexible until the end of March as to what extent the meeting can be held online.
As the chair of the Congress Committee, I cordially invite you to join the 25th World Congress of Neurology (WCN) to be held Oct. 3-7, 2021, in Rome, Italy. Since the pandemic of COVID-19 will not completely fade out by then, we are most likely to have a hybrid-type congress, providing you the option of attending in person or virtually. The committee has decided that we will remain flexible until the end of March as to what extent the meeting can be held online.