By JMS Pearce MD, FRCP
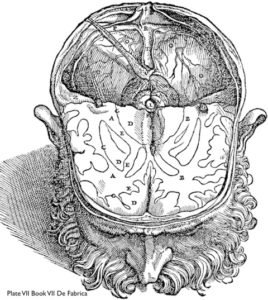
Plate VII, Book VII, Vesalius’s ‘De Fabrica’ from https://www.researchgate.net/figure/Andreas-Vesaliuss-depiction-of-the-basal-ganglia-This-reproduction-of-plate-VII-of-book_fig1_276048418
In his De Humani Corporis Fabrica (1543), anatomically Andreas Vesalius distinguished the subcortical nuclei of the corpus striatum from the cortex and white matter, but he neither named them nor suggested their possible functions.
The corpus striatum was named by Thomas Willis (1621–1675), (whose birth quatercentenary we celebrate this year) in Cerebri Anatome (1664). He believed it was the source of motor functions, a view that persisted for almost 200 years.
The German anatomist and physiologist Karl Friedrich Burdach (1776-1847) provided more anatomical detail, but he had little idea about function, believing that the basal nuclei were responsible for sensory perception and consciousness. However, he differentiated the caudate nucleus (Streifenhügel) from the putamen (Schale). He also identified the substantia nigra (schwarzgraue), and the pale inner part of the lentiform nucleus that he called globus pallidus.
Before 1870, the motor function of the corticospinal pyramidal tract and the existence of an extrapyramidal system were not understood. The brain was simply the organ of consciousness, memory, and intelligence. The cortex was not known either to control or initiate motor function, not least because anatomists had not clearly delineated the anatomy or the physiology of the several descending tracts.
Electrophysiologically, Gustav Fritsch(1838-1927) and Eduard Hitzig (1838-1907) first showed the role of the pyramidal system, i.e. the motor cortex and its efferent tracts, in 1870. David Ferrier’s (1843-1928) classical ablation/stimulation experiments extended the results of Fritsch and Hitzig. He showed that Faradic stimulation of the cerebral cortex could produce movements and fits, and that cerebral functions were localized in definable discrete areas, which he mapped as sensory and motor across several species, thus defining cerebral localization. Carpenter in 1874 ranked Ferrier’s cerebral localization “among the greatest advances in the physiology of the nervous system made in the last 50 years.”
As a concept, the extrapyramidal system (EPS) was first conceived indirectly by Johann Prus (of Lemberg, Galicia, now Lviv, Ukraine) in 1898. He discovered that experimental lesions in the pyramidal tracts failed to control induced cortical epilepsy. He unilaterally transected the pyramidal tract in dogs at the levels of the internal capsule, midbrain, pons, and medulla, and noted:
“Bilateral epileptic seizures occurred on stimulation of the cerebral cortex, on the same as well as the side opposite the operation… To explain the results of my experiments I had to assume that there is in the dog either bilateral innervation in the cortex, and that excitation spreads to the other hemisphere by means of the commissure fibres when the pyramidal tract has been cut, or that in this case conduction of cortical epilepsy takes place by means of a so far unknown centrifugal, i.e., motor pathway (Italics by JMSP).”
He deduced the presence of an unknown centrifugal motor pathway. But it was Samuel Kinnier Alexander Wilson (1878-1937) who was first to use the term “extrapyramidal” in its modern sense. His term extrapyramidal was adopted to distinguish between the clinical effects produced by damage of the basal nuclear tracts and those caused by damage to the classic pyramidal pathway.
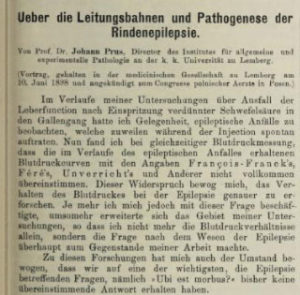
Prus‘s 1898 publication in the Wiener klinische Wochenschrift
In his 1912 classic paper Progressive Lenticular Degeneration (Wilson’s disease), he described the autopsy of three patients with this disease where he observed pathology outside the pyramidal system and named them extrapyramidal tracts:
“In spite of the great degree of motor weakness and helplessness, in a pure case [of hepatolenticular degeneration] the abdominal reflexes are preserved and a double flexor response is obtained. … the problem lay outside of the pyramidal system, “ in other words, this affection, where it occurs in an uncomplicated form, is an extrapyramidal motor disease. … To distinguish these apparently motor pathways from pyramidal and pontine tracts we shall call them extrapyramidal tracts.”
Although he failed to define specific tracts anatomically, this was the first use of the term “extrapyramidal” in neurology literature. In this era, several others inferred a motor role for areas outside the pyramidal tracts. (See Table 1.) The Swiss neurologist (of Russian descent) Constantin von Monakow (1853-1930) delineated a rubrospinal tract and the Austrian neuropsychiatrist Baron Constantin von Economo (1876-1931) proposed that the substantia nigra was involved with motor control of chewing and swallowing; lesions of the substantia nigra and red nucleus of cats and monkeys induced choreoathetosis. The Russian neurologist Vladimir Bechterew (1857-1927) stimulated the substantia nigra in dogs and noted swallowing, changes in respiration, ocular and pupillary changes, and contraction of neck muscles.9
Before Wilson’s paper, the confusion about sites of pathology in the several extrapyramidal disorders is evident in James Parkinson’s (1755-1824) account of the disease he discovered in 1817; he mistakenly guessed it originated in the “medulla spinalis.” The pathology was then unknown, but in 1894 while studying paralysis agitans, Hermann Oppenheim (1858-1919), the foremost Berlin clinical neurologist, provided sufficient clinical evidence to establish the duality of motor control, and to infer the existence of both pyramidal and extrapyramidal tracts in motor function. He wrote:
“Resistance to passive motion is always present in the later stages, and often before that time. It differs from spastic rigidity [of pyramidal tract disorders] in that it is not increased by passive motion, but is constant and regular . . .”
William Alexander Hammond (1828-1900), a founder of American Neurology in A treatise on diseases of the nervous system of 1871 recognized athetosis and suggested: “One probable seat of the morbid process is the corpus striatum.” The Austrian neuropsychiatrist Gabriel Anton (1858–1933) in 1896 indicated the basal nuclei could cause a motor disorder when in childhood double athetosis he reported hypermyelinated lesions in the putamen, later named état marbré,
Wilson’s long classic paper11 pointed out that the EPS (extrapyramidal system) had a “steadying” influence on the anterior horn cells:
“the relation of the corpus striatum (basal ganglia) to the rest of the motor system is one of tone control, and of steadiness of innervation. . . . Remove its influence by disease, [then] tonic postures become overemphasized.”
His view of dual motor function, pyramidal and extrapyramidal, was quickly and widely accepted.
Extrapyramidal Disease
The term extrapyramidal disease now refers to a group of motor disorders associated with pathological alterations in the basal grey matter whose function is predominantly motor. Clinically, extrapyramidal disorders consist of one or a combination of the following phenomena:
- abnormal involuntary movements
- changes in tone of skeletal muscles with an increase or decrease in resistance to passive motion
- poverty or excess of movement
- alteration of automatic movements.
The two motor systems are linked both anatomically and functionally, with extensive feedback loops.
Anatomically, the striatal EPS is polysynaptic and consists of nuclei and fibre tracts that receives projections from the cerebral cortex and sends efferent subcortical pathways to the brainstem and cord. Extrapyramidal structures comprise the cerebellum, basal nuclei including the neostriatum — subcortical caudate nucleus and the putamen nuclei — plus the substantia nigra, red nucleus, and the subthalamic nucleus of Luys. From them arise subcortical extrapyramidal tracts that terminate in the spinal cord. The Tectospinal, rubrospinsal, reticulospinal, and vestibulospinal tracts were described within the two decades 1890-1910.
Functionally, the EPS maintains posture and regulates involuntary postural tone and movement. It also has a role in behaviour, learning and cognition. Medium spiny neurons are the principal neurons of the striatum. They are the efferent cells, projecting to both segments of the globus pallidus, ventral pallidum, and substantia nigra. GABAergic in function, they are of several subtypes, and contain dopamine receptors and cholinergic and GABAergic interneurons. Both pyramidal and extrapyramidal systems project in the descending white matter tracts. (See Table 1.)
The extrapyramidal motor disorders are well recognized in basal nuclear diseases. They include Parkinson disease, Huntington chorea, Sydenham chorea, multiple system atrophy, torsion dystonias, and progressive supranuclear palsy. Altered posture and tone generally accompany involuntary movements, both bradykinetic and hyperkinetic — recognizable as tics, tremors, myoclonus, ballistic movements, chorea, and athetosis. They often show clinically characteristic individual patterns.
Exhaustive classifications (ICD-10 codes G20-G26 Chapter VI): contain 38 pages that include: acute dystonic reactions, blepharospasm, neuroleptic malignant syndrome, oculogyric crises, akathisia, drug-induced Parkinsonism, and various dyskinesias. •
JMS Pearce MD, FRCP, is Emeritus Consultant Neurologist at the Department of Neurology, Hull Royal Infirmary. E-mail: jms.pearce@me.com
References
-
Parent A. The History of the Basal Ganglia: The Contribution of Karl Friedrich Burdach. Neuroscience & Medicine 2012;03: 374-379. 10.4236/nm.2012.34046.
-
Quatercentenary of Thomas Willis’s birth — Department of Physiology, Anatomy and Genetics (DPAG) (ox.ac.uk)
-
Burdach KF. Vom Baue und Leben des Gehirns (Of Structure and Life of the Brain);1819 -1826. cited by Parent1
-
Lanska DJ. Early Controversies over Athetosis: I. Clinical Features, Differentiation from other Movement Disorders, Associated Conditions, and Pathology. Tremor Other Hyperkinet Mov (N Y). 2013;3:tre-03-132-2918-1.
-
Pearce JMS. Sir David Ferrier MD, FRS. J Neurol Neurosurg Psychiatry. 2003 Jun;74(6):787.
-
Ferrier D. The Functions of the Brain. London: Smith, Elder, 1876, pp. 163-196. [dedicated to Hughlings Jackson.]
-
Carpenter W. On the Physiological Import of Dr. Ferrier’s Experimental Investigations into the Functions of the Brain, West Riding Lunatic Asylum Med Reports 1874; 4: 1-23.
-
Prus J. Ueber die Leitungsbahnen und Pathogenese der Rindenepilepsie [Pathways and pathogenesis of cortical epilepsy] Wiener Klinische Wochenschrift, 11 (1898), pp. 857-863 (Annotated translation by Willner & Kennard, 1948
-
Louis ED. The Origins of the Term “Extrapyramidal” within the Context of Late Nineteenth- and Early Twentieth-Century Neurology, Neurophysiology and Neuropathology. The Journal of the History of Medicine and Allied Sciences, 1993. pp. 68-79
-
Lee J, Muzio MR. Neuroanatomy, Extrapyramidal System. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020.
-
Wilson S.A.K., Progressive lenticular degeneration: A familial nervous disease associated with cirrhosis of the liver. Brain, 1912, 34, 296-509.
-
von Monakow C. Der rote Kern, die Haube und die Regio hypothalamica bei einigen Säugetieren und beim Menschen. Arb. Hirnanat, Inst. Zurich, 1909, 3, 49—267.
-
von Economo C J. Zur Physiologie und Anatomie des mittelhirns. Arch. Psychiat. Nervenkr 1910; 46, 275-356;
-
Schiller F. The Vicissitudes Of The Basal Ganglia (Further Landmarks in Cerebral Nomenclature). Bulletin of the History of Medicine
-
1967;41:515-538.
-
Oppenheim H. Lehrbuch der Nervenkrankheiten. Berlin S. Karger 1894. translated 2nd edn : Textbook of Nervous Disease. New York, G. E. Steckert, 1911.
-
H. McDowdl and J. M. Cedarbaum, in Clinical Neurology, eds. A. B. Baker and R. J. Joynt (Philadelphia:]. B. Lippincott Company, 1990), pp. 1-97.
-
Goetz T, Arslan A, Wisden W, Wulff P. GABA(A) receptors: structure and function in the basal ganglia. Prog Brain Res. 2007;160:21-41.
-
Lanska DJ. Nhe history of movement disorders. Handbook Clinical Neurology. Chapter 33. 2010;95:501-46.