Given the relative simplicity of the conditions, which did not require a complicated experimental set-up, the obstacle lay only in the unfortunate predominance of rigid doctrines, which distorted the bare facts and arbitrarily remodeled them in favor of vague speculations. Only in this way could it come about that for a time the brain could be denied any movement and that the dura mater was elevated to the most important of all parts of the body, the meninges to the seat of all ability to move and to erapture.
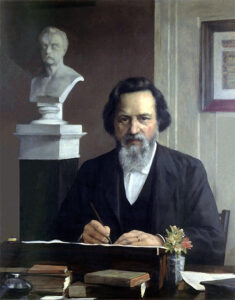
Max Neuburger, 1897

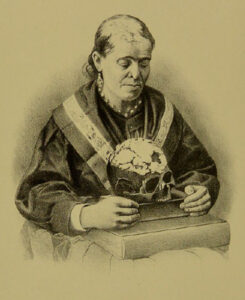
Italian anatomist Antonio Pacchioni
By Peter J. Koehler, MD, PhD, FAAN
This citation is from a chapter on “Versuche an der harten Hirnhaut und über Hirnbewegung” [Experiments on the Dura Mater and on Brain Movement] in the book Die historische Entwicklung der experimentellen Gehirn- und Rückenmarksphysiologie vor Flourens [The historical development of experimental brain and spinal cord physiology before Flourens] by Austrian physician and medical historian Max Neuburger (1868-1955).1 Naturalists have thought about and done experiments with respect to brain movements at least since Galen of Pergamon (129-216 CE). They wondered about the relation between the function of the brain and its movements. These movements could be observed in cranial wounds, as was described in the Edwin Smith surgical papyrus almost three millennia BCE, but also in children while the fontanel was still open, which was probably already noted by Pliny (23-79 CE). Most neurologists will have observed the movements indirectly, when doing a lumbar puncture and measuring the pressure in a plastic tube. In this essay, I will provide some historical information about this subject.
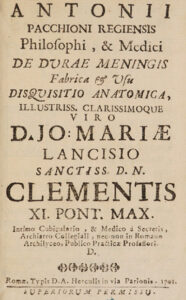
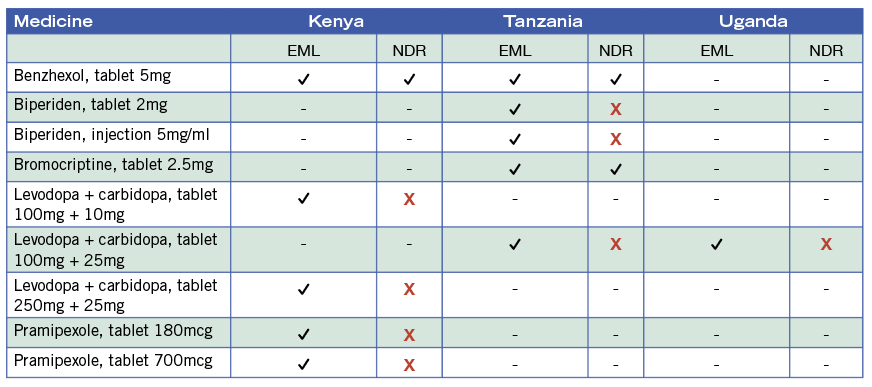
Pacchioni’s publication (1701)
Galen
Galen opined that the whole brain moved and had a systole as well as diastole. The movement was believed to be related to respiration. Air was thought to enter the ventricular system by the nose and cribriform plate of the ethmoid bone during inhalation, thereby expanding the brain. During exhalation it would leave the brain again. This had a dual function, including the driving of animal spirits from the ventricles into the nerves and the perception of smells. Interestingly, several physicians related the swelling and collapse of the bulging brain in cranial trauma to the phases of the moon, an idea that seems to have lasted for a long period.1, p.71 As is true for so many of Galen’s ideas, the dual function continued to be relied upon by physicians for many centuries, including Bauhinus (Gaspard Bauhin 1560-1624) and Carolus Fracassatus (Carlo Fracassati 1630-1672).

Giorgio Baglivi
Muscular Dura Mater or Brain Proper?
Two lines of ideas developed with respect to the origin of brain movements. One group of naturalists believed it was caused by the movements of the dura mater, the brain itself moving only secondarily. Others believed it was due to movement of the brain proper. Indeed a contractile power was assigned to the dura mater by Italian anatomist Antonio Pacchioni (1665-1726), who was interested in particular in the dura mater (De durae meningis fabrica et usu disquisitio anatomica [An anatomical discussion of the structure and use of the dura mater]).2 He became well-known by the eponym Pacchioni’s or arachnoid granulations.
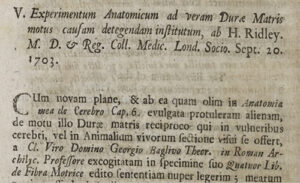
Report of Ridley’s paper at the Royal Society (1703)
When studying the dura mater, after boiling it, he was able to demonstrate a radiating arrangement of its fibers in the form of pyramids. He thought this structure consisted of three muscles and four tendons.3, p. 77 He compared the arrangement of the fibers with the chambers of the heart and recognized a double movement. At one moment, the cerebrum was compressed and the cerebellum became free. At the following moment, the situation would be the reverse. In this way, these muscles were responsible for transport of blood to the brain and the circulation of the nervous juice, like the heart had its function for the circulation of blood.
His colleague Giorgio Baglivi (1668-1707) elaborated upon this idea and supposed that the heart pushed the blood into the brain causing it to distend. The dura mater would then contract and push the nervous fluid into the nerves. In this way, he suggested two hearts and named the dura mater cor cerebri.3, p.7 In fact he attributed the highest control center to the dura mater, which he considered a vital structure.1, p. 77 These ideas proved very successful and were accepted by many anatomists and physicians, including Giovanni Maria Lancisi (1654-1720), Friedrich Hoffmann (1660-17420, Giovanni Domenico Santorini (1681-1737), and in particular Georg Ernst Stahl (1659-1734).

Jan Daniel Schlichting
Respiration
The English physician Humphrey Ridley (1653-1708), who graduated from Leiden with a dissertation De lue venerea (1679), may have been among the first to prove that destruction of the dura mater did not cease the movements of the brain. He read his paper at the Royal Society in 1703: “Experimentum anatomicum ad veram durae matris motus causam detegendam institutum” [An anatomical experiment to discover the real cause of the movement of the dura mater].4 Even more convincingly it was proved by the Dutch physician and anatomist Jan Daniel Schlichting (1703-1765), who studied medicine in the Dutch cities of Leiden and Groningen before he settled in Amsterdam. In his “De motu cerebri” he reported on his experiments, carried out upon several kinds of animals (dogs, cats, and rabbits), that brain movements remain after removal of the dura mater. “We solve, therefore, the problem that learned men have created for themselves by saying that the dura mater contracts and relaxes or pulsates”.
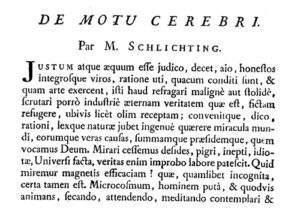
Schlichting’s 1750 article
He related the movements with breathing: “Every time a man breathes out, the entire brain rises up, that is, swells, and every time he breathes in, it goes down, that is, it subsides”.5 Thus he mentioned the opposite of what Galen had asserted 1,500 years previously. However, Schlichting did not know whether the swelling up during expiration was due to an increase influx of blood, by the increased air pressure, or by both.1, pp. 82-3 His experiments were repeated and the conclusions largely confirmed by the French physician Anne-Charles Lorry (1726-1783), stating that “The ancients followed their presumptions when they thought that the brain swelled up in time with inspiration: M. Schlichting is indeed supported by observation when he claims that it is synchronous with expiration”.1, p.84 However, Lorry believed the movements were only present in extraordinary conditions, like respiratory obstruction, pathological states, and cranial defects. He was one of several physicians, who denied brain movement to exist in normal conditions.

Jan Daniel Schlichting
The Swiss physician and physiologist Albrecht von Haller (1708-1777) was also among the physicians to refute the Pacchioni-Baglivi concept about the function of the dura mater. He confirmed the elevation of the brain during expiration and sinking down during inspiration. He related this to the venous congestion and outflow. However, it remained a matter of debate how that occurred. Some attributed the movements to the action of the heart, others to that of the influence upon the venous return of blood by breathing, and a third group believed that a combination of the two was responsible.

Anne-Charles Lorry
Brain Proper Moves Synchronously With the Heart
Several physicians observed that the brain moves synchronously with the heart. Among them were some well-known persons including the Italian anatomist and surgeon Realdus Columbus (Matteo Colombo c. 1515-1559), the French anatomist Jean Riolan (1580-1657), the Dutch physician IJsbrand van Diemerbroeck (1609-1674), Ridley, the French anatomist Raymond Vieussens (1641-1715), Haller and Marie-François-Xavier Bichat (1771-1802). However, there were various opinions on how the heart could move the brain. Several, including Bichat, believed it being the effect of the arterial pulse. Others were still denying such a synchronous movement. Marie-Jean-Pierre Flourens (1794-1867), for instance, denied a pulsating movement of the brain, only confirming a synchronous movement with respiration.
Franciscus Cornelis Donders
The German anatomist and anthropologist Johann Alexander Ecker (1816-1887), who summarized the history of brain movements, experimented with animals and concluded that there is a double movement in human beings and mammals, notably with the heart and respiration. The pulsating movement, he believed, was due to the arteries at the base of the brain as well as their branches in the brain parenchyma. He attributed the respiratory movement to the influx into the ventricles of cerebrospinal fluid (CSF) during expiration, although the venous filling in the brain may contribute to it.3, p.123

Ernst von Leyden
Spying on Nature Directly
At the time, some physiologists were more critical about the influence of the CSF. Writing on the results of his experiments, the Dutch physiologist and ophthalmologist Franciscus Cornelis Donders (1818-1889) mentioned that “the CSF is the condition, not the cause of brain movement.” Trying to answer the question whether brain movements exist when the skull is completely closed, he denied any movements of the brain if the skull was closed. The source of the question derived from two observations. Ecker believed the movements continued, whereas Johannes Müller declared that this was physically impossible.6 The French anatomist and physiologist François Achille Longet (1811-1871), based on observations published in Bourgougnon’s 1839 dissertation, also denied brain movements with closed skull. “Sans doute il est curieux de rechercher pourquoi le cerveau se meut chez les animaux trépanés; mais il est, suivant nous, bien plus important de savoir si ces mouvements préexistent à la trépanation” [No doubt it is curious to investigate why the brain moves in trepanned animals; but it is, in our opinion, far more important to know whether these movements pre-exist trepanation]. A comparison was made with the movements of the lungs that are quite extensive when the thoracic cage is opened, in comparison to the much less extensive movements in the physiological situation. Longet considered experiments to research brain movements, during which the skull was opened as useless. Therefore, Donders decided to open the skull of a rabbit. “I managed to spy on nature directly. When the skull is closed I have not only observed immediately and life, what concerns the brain movements, but also the increased and decreased supply of blood, with changes in blood pressure.” After trepanning the skull and removing a small part of the dura mater, he inserted a small glass window. “Through the small glass window one could observe the brain perfectly well, but we saw no trace of movement.7 I now amplified the inhalation and exhalation excursions by keeping the mouth and nose closed. Repeatedly again no movements.” At last, the small glass came loose, after which both types of movement, respiratory as well as circulatory, returned. The experiment was witnessed by several of his colleagues. After bonding the glass in the opening again, he did not observe any movements anymore and was able to see it for more than eleven days, sometimes using a loupe and even a microscope. He repeated the experiment several times and had special watch glasses made for the purpose.

Angelo Mosso
From Brain Movements to Intracranial Pressure
Still working in Königsberg (the present Kaliningrad), the German physician Ernst von Leyden (1832-1910) did important research on brain movements and in particular on intracranial pressure, which he published in 1866.6 He confirmed Donders’ observations, but instead of rabbits he used dogs, in which brain movements are clearer. Next to a small glass window, he inserted a lockable pipe, so that he could easily open and close the hole in the skull. He realized that the pressure waves by respiratory and circulatory movements with the tap locked would be borne by the brain. Like Victor von Bruns (1812-1883), Von Leyden tried to represent the changes in a graph, but encountered too many difficulties to show the movements due the low force that cause them. However, he was able to show the respiratory and circulatory quite nicely, by using a barometer tube filled with water. The rest of his long research paper is about measuring intracranial pressure under normal circumstances as well as with pathologically increased pressure.8
Catherina X (from Mosso10)
Registrations in Patients
About 10 years later in Turin, Carlo Giacomini (1840-1898) in cooperation with the well-known physiologist Angelo Mosso (1846-1910), were able to register brain movements by using an instrument developed by the French physiologist Etienne-Jules Marey (1830-1904; “méthode graphique”). They published their paper in the first volume of Archivio per le Scienze Mediche. The recordings were done in the open skull of the 37-year Catherine X, who suffered from syphilis. Despite years of treatment with potassium iodide and mercury ointment, the skull became affected and the researchers were able to observe the pulsations of the dura mater synchronously with the heart beats.9 In Mosso’s 1881 monograph Kreislauf des Blutes im menschlichen Gehirn [Circulation of the blood in the human brain], we find a drawing of Catherine and her skull.10 Giacomini’s and Mosso’s paper was read at the Académie in Paris by no one less than the famous physiologist Claude Bernard (1813-1878),11 who informed the audience that at the time the patient had been completely cured.
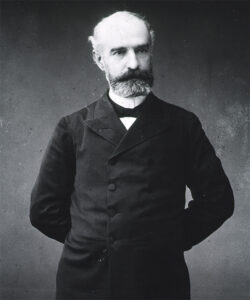
Charles-Emile François-Franck (National Library of Medicine; Digital Collections. Public domain)
Not long after the Italian publication, the French physiologist Charles-Emile François-Franck (1849-1921), a pupil of Marey, was able to register the brain movements of a similar case. He was aided by young Edouard Brissaud (1852-1909; described geste antagoniste in dystonia), who made the registrations and was allowed, at the end of the article, to present the case history. It was about the 34-year old Victoire All… , who suffered from syphilis, for which she was treated with liquor swietenii, a mercury based mixture that was introduced the previous century by Gerard van Swieten (1700-1772). The dosage of mercury was lower than that applied earlier. However, the skull became affected and parts needed to be removed, providing access to the researchers.
At the end of the 19th century, British physiologist Leonard Hill (1866-1952) summarized the literature on the subject, in particular the decades before his book was published. Referring to “Althan,” probably the Estonian born Georg Althann (1839-1898), he noted that “the errors of Donders … arose from the neglect of the fact that the brain pulsates in a direction where resistance is least. Thus when the cranium is trephined and the dura opened, the pulse can scarcely be seen in the occipito-atlantal membrane, for the trephine hole has now become the seat of least resistance. Similarly, when a trephine hole is closed by a glass window, the occipito-atlantal membrane becomes the seat of least resistance, and a pulsation appears there.”12, p.8-15
Today the pulsating brain still is an area of research in particular with respect to the effects on MRI scans and more recently the concept of the glymphatic system. Arterial pulsations are thought to drive flow through perivascular spaces for clearance of metabolic waste.13 •
References
1. Neuburger M (1897). Die historische Entwicklung der experimentellen Gehirn- und Rückenmarksphysiologie vor Flourens. Stuttgart, Enke. English edition transl. and edited by Edwin Clarke The historical development of experimental brain and spinal cord physiology before Flourens. Baltimore/London, Johns Hopkins University Press.
2. Pacchioni A (1701). De durae meningitis fabrica et usu disquisition anatomica. Rome, Herculis.
3. Ecker A (1843). Physiologische Untersuchunge über die Bewegungen des Gehirns und Rückenmarks : insbesondere den Einfluss der Cerebrospinalflüssigkeit auf dieselben. Stuttgart, Schweizerbart.
4. Ridley H (1703). Experimentum anatomicum ad veram durae matris motus causam detegendam institutum Phil Trans 23, no. 287: 1480-4.
5. Schlichting JD (1750). De motu cerebri. Mémoires de Mathématique et de Physique (Paris) : 113-35.
6. Leyden E (1866). Beiträge und Untersuchungen zur Physiologie und Pathologie des Gehirns. Virchows Arch 37:519–559.
7. Donders FC (1850). De bewegingen der hersenen en de veranderingen der vaatvulling van de Pia Mater, ook bij gesloten onuitzetbaren schedel regtstreeks onderzocht. Nederlandsch Lancet, March/April, 521-53.
8. Koehler PJ, Wijdicks EF (2015). Fixed and dilated: the history of a classic pupil abnormality. J Neurosurg;122:453-63.
9. Giacomini C, Mosso A (1876). Esperienze sui movimenti del cervello nell’uomo. Archivio per le Scienze Mediche 1:245-78.
10. Mosso A (1881). Kreislauf des Blutes im menschlichen Gehirn, Leipzig, Veit, p. 223
11. Giacomini C, Mosso A (1877). Etude graphique des mouvements du cerveau de l’homme. C R Académie Sciences (Paris) 24 : 41-3.
12. Hill L (1896). The Physiology and Pathology of the Cerebral Circulation: An Experimental Research. London: Churchill.
13. Mestre H, Tithof J, Du T, Song W, Peng W, Sweeney AM, Olveda G, Thomas JH, Nedergaard M, Kelley DH (2018). Flow of cerebrospinal fluid is driven by arterial pulsations and is reduced in hypertension. Nat Commun 9:4878.