Prof. Wolfgang Grisold provides updates on the Council of Delegates, regional societies, and global activities.
For this column, I would like to update you on the upcoming Council of Delegates (COD) meeting, the joint meeting of the Japanese Society of Neurology, and the Asian and Oceanian Association of Neurology (AOAN) in Japan, as well as report on other global activities.

From left to right: Queen Mathilde of Belgium, Elena Moro, EAN president-elect, and Claudio Bassetti, EAN past -president.
Council of Delegates Meeting (COD)
Each year, the World Federation of Neurology (WFN) holds its COD meeting, which is the formal organizational meeting of the WFN. Preceding this meeting, all WFN procedures and activities from 2023 are audited and submitted to the delegates. This includes all activities and financial transactions, which are provided in a report. The trustees are responsible for this important document and will be available for questions and answers.

Carlayne Jackson, AAN president, (foreground), and Tarun Dua, head of the WHO brain health unit, are taking notes.
This year’s COD meeting will be held virtually, including the virtual election of one trustee. The experience of the past few years as well as the increasing challenges with travel have made these virtual meetings the best choice.
At the upcoming meeting, the elected trustee position held by Alla Guekht for two terms will need to be filled. The Nomination Committee, which acts independently from the trustees, has selected six candidates from Asia, Europe, and Latin America. The committee considers these candidates as equal and does not indicate any preference. Thus, it will be on the shoulders of the delegates to review the candidate presentations. These are available on the WFN website and on page 15 of this issue. The election details will be communicated to the delegates, the voting will be conducted electronically, and the elected trustee will be presented at the trustee meeting.
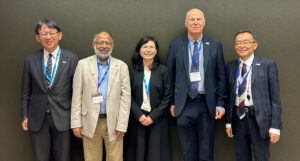
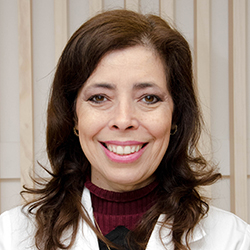
Leadership Meeting with the Japanese Society of Neurology. (from left to right) Prof. Ryosuke Takahashi, Prof. Mohammad Wasay, Prof. Ritsuko Hanajima, Prof. Wolfgang Grisold, and Prof. Yoshikazu Ugawa.
There will also be reports from the president, vice president, treasurer, secretary general, and several committees. We also expect an update on preparations for WCN 2025, which will be hosted in Seoul, South Korea. The site of WCN 2027 will be Cape Town, South Africa. WCN 2029 will be in Europe. The call for candidate cities will be made soon.
We are pleased to announce the International Congress of Neuromuscular Diseases (ICNMD) 2024, which will take place in Perth, Australia, and will follow the successful series of WFN ICNMD Congresses. The newly introduced World Federation of Neurology Update (WNU) virtual congress will take place Sept. 26-27.
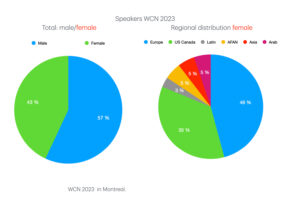
Figure 1. Speaker distribution at the World Congress of Neurology (WCN) 2023 in Montreal by gender and region. While the distribution of speakers approaches an equal distribution, the regional participation of female speakers is dominated by Europe and North America.
Regional Societies
We recently participated in the AAN meeting in Denver and the Japanese Society of Neurology and AOAN meeting in Japan. We look forward to the European Academy of Neurology (EAN) meeting in Helsinki as well as the African Academy of Neurology (AFAN) meeting in Dakar. The WFN uses these opportunities to participate and communicate with leadership and delegates. We also hosted booths to present information about the WFN, the WCN, and the ICNMD.
The EAN organized its Brain Health Summit May 7 in Brussels and addressed many aspects of brain health. Several important European health analyses on neurological disease as well as an analysis of needs and costs were presented. Queen Mathilde of Belgium attended the sessions and held an animated discussion with the faculty during the coffee break. The EAN provided an impressive demonstration of how to raise the matter of brain health to higher political levels.
The joint meeting of the Journal of Neurological Sciences (JNS) and the AOAN took place May 29-June 2 in Tokyo, and included a leadership meeting with the JNS and the WFN, represented by Mohammad Wasay and Wolfgang Grisold, who were privileged to attend the AOAN delegate meeting. Hamidon Basri stepped down as the AOAN president, and Christopher Chen (Singapore) will serve as the new AOAN president. I want to thank Prof. Basri for his service in the past years, and I look forward to him continuing to work with the WFN.
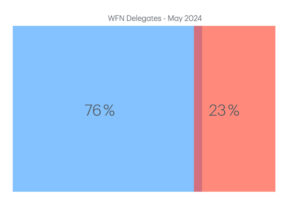
Figure 2. Gender distribution of WFN delegates. This is similar to the worldwide distribution of parliamentarian members.
The WFN continues its efforts to participate in worldwide activities on brain health, as well as advocate for the importance of the Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders (IGAP). It also excited about the upcoming presentation of the WHO IGAP toolkit, which will be available July 8. Prof. Grisold stressed the importance for member societies engaging with this important WHO initiative to promote and advocate for brain health and the IGAP.
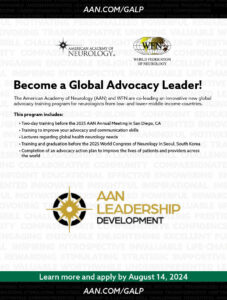
The WFN has entered into a joint initiative with the AAN. Called the Global Advocacy and Leadership Program (GALP), this unique program is designed to provide young neurologists in low- and middle-income countries around the world tuition for live, in-person courses on advocacy and leadership in San Diego (AAN) and Seoul (WCN) as well as a series of virtual sessions in between. Graduation will be held at the Seoul congress. This joint AAN-WFN activity will increase the potential of young neurologists to advocate for neurology as well as increase the awareness for advocacy and leadership worldwide. The applications will be announced by the AAN and WFN in July 2024.
The JNS meeting was perfectly organized, and the JNS now has 10,000 members. The WFN was invited to participate in a session on gender and diversity issues, and received input from speakers from Canada, Japan, and Malaysia, giving regional insight into these important aspects.
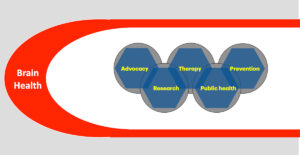
Figure 3. Brain health is a powerful envelop to promote neurology worldwide. Embedded is the IGAP and its five pillars.
The gender distribution worldwide for WFN delegates is 77% male and 23% female. The speaker distribution in Montreal (WCN 2023) was 57% male and 43% female. The membership in WFN committees and subcommittees is 53% male and 47% female. Worldwide, the distribution of parliamentarian members is approximately 75% male and 23% female; the distribution of WFN delegates is similar. But we have been more successful with the distribution in the committees and speakers. Our goal will be a 50/50 distribution. We congratulate the JNS for the organization of this important session.
The highlight for the WFN presence was a session on global neurology with a discussion of the IGAP. WFN speakers were Wolfgang Grisold, Mohammad Wasay, and Tissa Wijnerate. The importance of brain health and the IGAP were emphasized by Prof. Grisold.
From Mongolia, a detailed lecture was given by neurologist Jambal Sarangerel. Prof. Augustina Charway Felli, from the AFAN, presented her lecture via recorded video. The ensuing discussion gave additional information on the purpose and content of the IGAP, and the impression was that the messages were well received.
Prof. Grisold was honored to be one of three speakers at the JNS delegates gala dinner. In addition to the recognition of the JNS and its excellent partnership over decades, he praised the late WFN past-president J. Kimura and past vice president Ruyji Kaji for their contributions to the WFN.

Ryosuke Takahashi (second from the right) invited the lecturers of the gender session (Lorraine Kalia, Isobe Noriko, Sonoko Misawa, Aihuey Tan, Wolfgang Grisold) to a traditional Japanese restaurant, where discussions could be continued.
“The world does not stop“ was his call to the delegates to take up brain health as well as to use the content of IGAP to advocate for neurology in the region.
The WFN was also present in the exhibition hall in two booths. The WFN shared one booth with Korea, which presented information about WCN 2025 in Seoul. The other booth featured the WFN International Congress on Neuromuscular Diseases (ICNMD), which will have its meeting this year in Perth, Australia. The booth was attended by Carlos Hunt from the WFN head office, and the ICNMD stand was attended by Alan Lee. Both stands distributed ample informational material.
The Latest Global Activities
The recent meeting at the U.N. ECOSOC Multistakeholder Forum on Science, Technology, and Innovation for the Sustainable Development Goals in New York was attended by Profs. Alla Guekht and Wolfgang Grisold, who delivered a statement on “Bridging the science, technology and innovation divides to eradicate poverty and end hunger.”

Some of the the AOAN delegates, from left to right: Dr. Hino, Dr. Thirugnam, Dr. Wiratman, Prof. Kim, Dr. Chung, Prof. Sambal, Prof. Lay, and Prof Ogawa.
This was well received and conveyed the importance of brain health.
On April 26, the high-level WHO Meeting to Defeat Meningitis took place in Paris.
It was under the patronage of French President Emmanuel Macron and was attended by WHO Director General Tedros Ghebreyesus. Impressive stories of patients made it clear to the audience that not only is fighting and defeating meningitis important, but a significant number of survivors suffer from disability. The actions and success of the WHO in this important task are impressive. The WFN is a stakeholder in this initiative and will help to bring this important information to our member societies.
The most important activity at present is the introduction of the WHO IGAP Toolkit, which will be released on July 8, 2024. This toolkit has been developed with support of the WFN, and is a well-balanced document that explains the implementation of the IGAP to all stakeholders. It is of extreme importance that this document, signed by all member states, will give neurologists a solid basis for discussing, implementing, and improving neurology services in their regions. The center of all activities are the persons affected.

Who Director General Tedros Ghebreyesus at the WHO Meeting to Defeat Meningitis.
The World Health Assembly took place in Geneva May 27-31. The WFN was represented by Profs. Alla Guekht and Ksenia Pochigaewa, who made statements on behalf of the WFN. Details of this meeting will be reported separately in World Neurology.
On July 22, World Brain Day (WBD) will be celebrated, and the theme is Brain Health and Prevention. Please see our website for information and the available material in our toolkit. Please use and modify the material to your needs and make your local society, and your country, aware of the importance of brain health and prevention. On July 22, please join us for an international webinar, with participants from the WHO and all WFN regions.

A special snow globe version of the WFN pin produced exclusively as a gift for the AAN leadership.
We look forward to your input and work for neurology worldwide. Last but not least, we congratulate Prof. Alla Guekht for her election as the incoming ILAE president.
WFN Pin
The WFN has created a new WFN pin. We will be glad to ship a pin and an IGAP information folder to the first 20 applicants before July 22, 2024. Please send your name, region, country, and professional role in your member society. Please also include comments on World Brain Day and the IGAP with a maximum of 500 words. Use the following address: info@wfneurology.org. The jury will select the most inspiring comments and use them for publication in an upcoming issue of World Neurology. •
In addition to this report and update on WFN developments and activities since the last edition, please follow our website and social media for more information. This year, the WFN launched a WFN service page in the (JNS). The third issue of the WFN service pages will contain information about the WFN core curriculum, the journal eNS, the WFN AFAN educational day, and the Italian Brain Health Initiative.



 The primary objective of the Italian Strategy is to create awareness about Brain Health throughout the country and start the implementation of initiatives to prevent and combat the development of mental and neurological diseases. The WHO IGAP provides a clear and precise map of actions that each country will need to take to optimize brain health.
The primary objective of the Italian Strategy is to create awareness about Brain Health throughout the country and start the implementation of initiatives to prevent and combat the development of mental and neurological diseases. The WHO IGAP provides a clear and precise map of actions that each country will need to take to optimize brain health.








 On the left, Christopher Luxon, Prime Minister of New Zealand, presenting the
On the left, Christopher Luxon, Prime Minister of New Zealand, presenting the