By Peter J. Koehler
The term eponym is derived from the Greek words epi- “sur” and onima “name.” It is hardly possible to imagine daily life without eponyms, although we are not always aware of using them. Just think of diesel engine, pasteurized milk, degrees Fahrenheit or Celsius, to name a few. Eponyms are found in nearly all sciences, including mathematics, astronomy, physics, chemistry, geography, paleontology, and botany (to mention a few: Pythagoras, Gödel, Fourier analysis, Avogadro).
The use of eponyms is not new. Carl Linnaeus (1707-1778) used them in botany. Other eponyms became verbs (galvanize, faradize) or units (watt, ampère, ohm, joule). The French “préfet” (prefect) of the Seine department Eugène-René Poubelle made the use of garbage cans obligatory, hence the French word “poubelle” for garbage can.
And what about the grenadier in Napoleon’s army, Nicolas Chauvin, who made propaganda for Napoleon following his return from the Isle of Elba in 1815 (chauvinism!)? A Dutch author estimated the number of eponyms in everyday language at 2,500-3,000. The Eponyms Dictionary Index features approximately 20,000 eponyms, including scientific eponyms.2
The choice of eponyms may tell something about the scientific evolution of the subject. Many eponyms in natural sciences, for instance, refer to persons from the 17th to 19th centuries, and the Scientific Revolution is supposed to have begun in the 17th century. As the scientific method in medicine was introduced in the mid-1800s, most medical eponyms find their origin after that period. Another interesting phenomenon to point to is that whereas 19th century eponyms are often single names, those from the late 19th and 20th century mainly consist of several names.2
Sources for Eponyms
Medical eponyms are derived from various sources. They are not only named after the discoverer of a disease or microbe who is honored (Borrelia Burgdorferi, Pick disease, Alzheimer’s). Sources also include mythical figures (Ondine’s curse, Oedipus complex), fairy tales (Alice-in-Wonderland syndrome), literature (Pickwick syndrome, Ophelia complex), artists (Brueghel syndrome), location (Lyme disease, Glasgow coma scale), and famous patients (Lou Gehrig).
An important source for finding the meaning of medical eponyms is www.whonamedit.com. The author, the Norwegian Ole Daniel Enersen, had the ambition to “present a complete survey of all medical phenomena named for a person,” with a short biography of that person.
Advocates and Adversaries
The use of eponyms is not generally accepted. There are adversaries and advocates. London neurologist William Gowers (1845-1915) wrote that “this system of nomenclature is full of inconvenience, increasing the difficulties of the student, and leading to frequent mistakes in scientific writings,” but he could not prohibit the use of his name in several eponyms4.
In his monograph on reflexes, Robert Wartenberg wrote that following the discovery by Joseph Babinski of the extensor plantar reflex, Wartenberg wrote about a plethora of discovered reflexes.
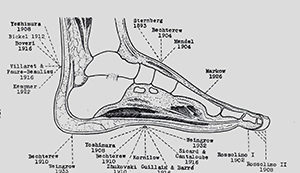
In his monograph on reflexes, Robert Wartenberg (1886-1956) wrote that following the discovery by Joseph Babinski (1857-1932) of the extensor plantar reflex (1896), a plethora of reflexes was discovered. The discoverers probably hoped to see their names immortalized. (See Figure 1.)5, p.93
The mania to associate eponyms to reflexes and phenomena was particularly endemic in Europe. Wartenberg was in favor of descriptive terms. However, descriptive terms also have disadvantages, for instance, when the understanding of phenomena or diseases change. Interestingly, he could not prevent the usage of his name for eponyms (e.g., Wartenberg sign for pyramidal involvement of the upper extremity).
A pro-con discussion on the use of eponyms was conducted some years ago in the British Medical Journal.6 The authors, who stated that the use of eponyms should be abandoned, provided several reasons, mostly quoting a short selection of rare, disputable eponyms. Of course, they were right proposing the deletion of eponyms connected with Nazi medicine. Larry Zeidman and colleagues have done research in this area during the past 10 years.7 The arguments that some eponyms may bring about confusion or do not refer to the original discoverer is often heard and probably true. The person writing in favor of eponyms provided more general arguments, including the opinion that the eponym “brings color to medicine,” “provides a convenient shorthand,” and are “embedded in medical traditions and culture in our history.” She expected eponyms would stay, despite the objections of some. Probably the shorthand and reference to the historical person are the most important arguments provided in favor of the use of eponyms.8
The Practical Use of Eponyms
Although done 20 years ago, a survey on neurological eponyms under Dutch neurologists (1997) provided interesting results. With 30 percent of the addressed members responding, a positive correlation was found between age of the responders and the knowledge of eponyms. The best-known eponyms were found in the category “tests and maneuvers.” Many of the responding neurologists and residents did not prefer descriptive terms above eponyms.9
In another paper on neurological eponyms, the author mentioned the confusion that may arise when it is not clear whether the eponym refers to a syndrome or a disease. Moreover, there is an evolution of some of the eponyms, as our understanding of disease processes expands.10 There is even an eponym about the doubts of the origin: Stigler’s law of eponymy states that “no scientific discovery is named after its original discover.”11
At least from a historical perspective, there is still interest in eponyms. Entering the term “eponym” in PubMed and limiting the search to “history of medicine” provides 1,034 hits. Adding “neurology” results in 121 hits. And how is the use of eponyms in textbooks? The index of a neurological textbook, Adams and Victor’s Principles of Neurology, counted 370 eponyms.12 Another example, Merritt’s Neurology, did not yield much less.13
Eponymous Women in Neurology
Many eponyms concern men. Even if the name refers to a woman, not everyone will realize this. In April 2017, Dr. Stephen Reich, current chair of the History Section of the American Academy of Neurology, organized a history course in which eight eponymous women in neurology were presented. In the following section, I will summarize them.

Augusta Dejerine Klumpke and her husband.
Dejerine-Klumpe Syndrome / Augusta Dejerine-Klumpke
Born in San Francisco, Augusta Dejerine-Klumpke moved to Paris, where she studied medicine, and, not without difficulties, she became the first female intern of the Paris hospitals. She married Jules-Joseph Dejerine in 1888. She described the work by which she was eponymized in 1885 in the Revue de Médecine.14 It is about lower trunk brachial plexopathy with hand weakness. It is commonly associated with oculopupillary phenomena (Horner’s syndrome). It is also referred to as Klumpke’s paralysis. (The paper was presented by Jennifer McKinney.)
Roussy-Lévy Syndrome / Gabrielle Lévy

Gabrielle Lévy
Born in Paris, where she studied medicine, Gabrielle Lévy became a pupil of Pierre Marie. She published on many subjects, the most important being post-encephalitic syndromes, which was also the subject of her 1922 thesis, and neuro-oncology, a subject she worked on when employed at the Paul-Brousse hospital that became an oncology center.
The eponym refers to a familial disease with gait problems, areflexia, and clubfoot (dystasie aréflexive héréditaire), today known to be caused either by a mutation in the PMP22 gene or the MPZ gene (as in the original family).15 Lévy died at age 48 from the disease that she had studied: a brain tumor or a post-encephalitic syndrome? (The paper was presented by Peter J. Koehler.)
Louis-Bar Syndrome (ataxia telangiectasia)/ Denise Louis-Bar
Denise Louis-Bar (originally Bar, she married civil engineer F. Louis) published (in French) a case of this multisystem disease (ataxia, ocular-cutaneous telangiectasias, and immune deficiency) at age 27 (1941).16 Born in Liège, Belgium, she studied medicine in Brussels and trained under Ludo van Bogaert, with whom she studied the first case in Antwerp. Boder and Sedgwick published on eight children from five families in recognizing the hereditary character (1958).17 Louis-Bar later worked at the internal medicine department in Liège and was known there as “la rousse medical” (the medical red-haired). (The paper was presented by Elisabeth A. Coon.)
Dix-Hallpike Maneuver / Margaret Dix

Margaret Ruth Dix
Margaret Dix (1902-1991) received her MD in 1957, after she had ended her career as a surgeon (she became a fellow of the Royal College of Surgeons in 1943), following an eye injury during the bombing of England in World War II. She became a neuro-otologist and trained with otologist Charles Skinner Hallpike. They worked at the otological research unit of the National Hospital for Neurology and Neurosurgery in London. Dix wrote many papers on several subjects, including the two classic papers on benign paroxysmal positional vertigo and the eponymous maneuver18,19. (The paper was presented by Douglas J. Lanska.)
Canavan Disease / Myrtelle May Canavan
Born in 1879 near St. Johns, Michigan, Myrtelle May Moore received her MD from the Women’s Medical College of Pennsylvania and married physician James Francis Canavan. She became interested in neuropathology, and from 1920 until her retirement in 1945, she worked as associate professor of neuropathology at Boston University and curator of the Warren Anatomical Museum at Harvard Medical School. She described the disease to which her name became attached in 1931,20 and it is now known to be an autosomal recessive neurodegenerative disease caused by a mutation in the ASPA gene resulting in aspartoacylase deficiency. Canavan died from Parkinson’s disease in 1953. (The paper was presented by Lenora Lehwald.)
Hurler Syndrome / Gertrud Hurler
Gertrud Hurler was born in 1889 in Rastenburg, Prussia, and went to medical school in Munich. She trained as a pediatrician under Meinhard von Pfaundler. She was given the cases of two brothers with dysmorphic features to study and describe. In addition, the children had developmental delays and clouded corneas. She recognized the hypotonia, cognitive impairment, short stature, macrocephaly, scaphocephaly, delayed anterior fontanelle closure, course facial features with prominent facial hair as well as the hepatoplenomegaly. Hurler published her paper in 1919.21 Despite a subsequent paper on the subject in 1920 by Von Pfaundler,22 the disease remained attached to her name. She was probably not aware of the publication by Charles Hunter, working in Winnipeg, Canada, who described two brothers without corneal clouding. When serving in Europe during World War I, he gave a presentation at the Royal Society of Medicine in London: “A rare disease in two brothers.”23 Frederick Parkes Weber (1863-1962), who was present at the meeting, concurred with the diagnosis of “gargoylism.” (The paper was presented by Margie Ream.)
Frey’s Syndrome / Lucja Frey

Lucja Frey
Following injury of the auriculotemporal nerve (for example, by parotid gland surgery; gunshot injury in the case of Frey’s patient), inappropriate regeneration may result in gustatory sweating (Frey’s syndrome). Lucja Frey was born in 1889 in Lvov, Poland. She attended medical school in the same city and following graduation, she worked under Kazimierz Orzechowski. She presented on the syndrome of the auriculotemporal nerve in Warsaw (1923) and published on it in a Polish as well as a French (Revue Neurologique) journal. 24 She published a large number of papers on various subjects. During the German occupation, she worked at the Lvov Ghetto Polyclinic and was killed in 1942. (The paper was presented by Stephen G. Reich.)
The Mary Walker Effect / Mary Broadfoot Walker
The Mary Walker effect is a curious observation presented in 1938 during a meeting of the Royal Society of Medicine.25 In myasthenic ptosis, the drooping of the eyelid can be reversed by prostigmin. When the effect of the prostigmin is wearing off, circulation in the arms is cut off by inflation of cuffs (to 200 mm Hg). Exercise of the forearms in this situation does not increase the ptosis. However, 1.5 minutes after the release of the cuffs, the ptosis increases and 2 minutes after the release general muscle weakness increases. Mary Walker believed that myasthenic muscles released a curarizing agent during activity, which passed into the bloodstream and blocked neuromuscular transmission elsewhere. Although her speculative idea was not correct, it stimulated the search for a circulating factor. She was the first to clearly demonstrate that strength temporarily improved in patients with myasthenia gravis when they were given physostigmine or neostigmine and published on this in 1934.26 The pertinent film clip may be found at www.youtube.com/watch?v=uRoRsmvkhTI.
Born in 1888 in Wigtown, Scotland, Mary Walker received a bachelor’s of medicine and bachelor’s of surgery degree from Glasgow and Edinburgh Medical College for Women in 1913. She became a member of the Royal College of Physicians in 1932 and received her MD from the University of Edinburg in 1935. She worked as a salaried Poor Law Service medical assistant at the Greenwich Union Infirmary/St. Alfege’s Hospital from 1920 to 1936 and several other hospitals after that. She died in 1974. (The paper was presented by Christopher J. Boes.)
Peter J. Koehler is based in Heerlen, Netherlands. More history is provided at his website at www.neurohistory.nl.
References
- This paper is based upon the Introduction of the 2008 AAN History Course “Eponyms in Neurology” (by PJK) and the 2017 AAN History Course “Eponymous Women in Neurology”.
- Arts NJM, Koehler PJ, Bruyn GW. Inleiding [Introduction]. Het neurologisch onderzoek in eponymen [The neurological examination in eponyms]. Nijmegen, Arts & Boeve, 1995, pp.1-10.
- Gowers WR. The diagnosis of diseases of the spinal cord. London, Churchill, 1880.
- Toodayan N, Boes CJ. The eponymous legacy of Sir William Richard Gowers (1845-1915):
A revealing letter. J Hist Neurosci 2017;26:169-192. - Wartenberg R. The examination of reflexes. A simplification. Chicago, The Yearbook Publisher, 1945.
- Woywodt A, Matteson E, Whitworth JA. Should eponyms be abandoned? BMJ 2007;335:424-5.
- Kondziella D, Zeidman LA. What’s in a Name? Neurological Eponyms of the Nazi Era. Front Neurol Neurosci. 2016;38:184-200.
- Koehler PJ, Bruyn GW, Pearce JMS. Neurological Eponyms. New York, Oxford University Press, 2000, p.v-vi.
- Franke L, Koehler PJ, Bruyn GW. The use of and familiarity with neurological eponyms at the close of the 20th century by Dutch neurologists. An inventory Clin Neurol Neuro¬surg 1997;99:91-8.
- Okun MS. Neurological eponyms – Who gets the credit? J Hist Neurosci 2003;12:91-103.
- Stigler SM. Stigler’s law of eponymy. In: Gieryn TF, ed. Science and social structure: a festschrift for Robert K. Merton. New York, NY Academy of Sciences, 1980.
- Ropper AH and Brown RH. Adams and Victor’s Principles of neurology (8th ed.) New York, McGraw-Hill, 2005
- Rowland LP (ed). Merritt’s Neurology (11th ed.). Philadelphia, Lippincott, Williams & Wilkins, 2005.
- Dejerine-Klumpke A.. Contribution à l’étude des paralysies radiculaires du plexus brachial. Paralysies radiculaires totales. Paralysies radiculaires inférieures. De la participation des filets sympathiques oculo-pupillaires dans ces paralysies. Revue de Médecine 1885, 5: 591-616, 739-90.
- Roussy G, Lévy G. Sept cas d’une maladie familiale particulière: troubles de la marche, pieds bots, et aréfléxie tendineuse généralisée, avec, accessoirement, légère maladresse des mains. Rev Neurol (Paris). 1926;33:427-50.
- Louis-Bar D. Sur un syndrome progressif cormprenant des télangiectasies capillaires cutanées et conjonctivales symétriques, à disposition naevoïde et des troubles cérébelleux. Confin Neurol 1941;4: 32-42.
- Boder E, Sedgwick RP. Ataxia-telangiectasia; a familial syndrome of progressive cerebellar ataxia, oculocutaneous telangiectasia and frequent pulmonary infection. Pediatrics 1958;21: 526-554.
- Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Proc Soc Med 1952;45:341-354.
- Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol 1952;61:987-1016.
- Canavan M. Schilder’s encephalitis perioxalis diffusa. 1931.
- Hurler, G. Über einen Typ multipler Abartungen, vorwiegend am Skelettsystem. Zeitschrift für Kinderheilkunde. Berlin. 1919;24: 220–234.
- Pfaundler M. Demonstrationen über einen Typus kindlicher Dysostose. Jahrbuch für
Kinderheilkunde und physische Erziehung, Berlin, 1920;92: 420. - Hunter CA. A rare disease in two brothers. Proceedings of the Royal Society of Medicine, London, 1917, volume 10, Section Dis. Children, 104-116.
- Frey L. Le syndrome du nerf auriculo-temporal Rev Neurol (Paris) 1923;2:92-104.
- Walker MB. Myasthenia gravis: a case in which fatigue of the forearm muscles could induce paralysis of extra-ocular muscles. Proc R Soc Med 1938;31:722.
- Walker MB. Treatment of myasthenia gravis with physostigmine. Lancet 1934;1:
1200–1201.
