By Richard Peatfield

Richard Peatfield
During the last 40 years, the world of headache has been blessed with two remarkable men: Dr. Seymour Diamond and Dr. Frank Clifford Rose. They have both recently published autobiographies. Rose’s autobiography is, of course, posthumous following his death in 2012, while Seymour, just the elder, is still enjoying his retirement at the age of 89.
Although living and working in different environments on different continents, Diamond and Rose have striking similarities over and above their lively personalities. They were born within 16 months of one another of Jewish immigrant stock. Rose’s parents settled in the East End of London after getting married and having two children in Romania. Rose was the youngest of seven surviving siblings.
Diamond’s parents, by contrast, had arrived in Chicago as children from Slovakia and from the Ukraine. He was the youngest of their four children. Both had that combination of inherent talent and industry that enabled them to move out of their original backgrounds.
I think it is fair to say that Rose’s path was advantaged by the grammar school and the university system of his time in Britain, while Diamond grew up in the challenging environment of wartime America. Never is this more clear than in their early clinical training. Rose was able to do all of his jobs within London, whereas Diamond tells the tale of his in-laws driving him, his new wife and all of their possessions from Chicago to Arkansas and then to Ohio every year or so.
Both spent the bulk of their careers as practicing physicians with interests in headache, though Diamond was never a board-certified neurologist as he had been accredited in family medicine and had not done a residency program in neurology.
Both set up dedicated migraine clinics. Rose’s clinic is dedicated to Princess Margaret, while Diamond’s bears his own name. Both wrote and edited a large numbers of books and conference proceedings.
Both were superb administrators and used their talents in a wider field. Rose was the more international, playing a major role in the evolution of the International Headache Society and serving as secretary treasurer general of the World Federation of Neurology.
Diamond, in contrast, devoted much of his energy to the inpatient and outpatient facility he established in Chicago and developed a nationwide reputation as a physician “who cared.” He was one of the first to try tricyclic antidepressants in headache patients and was the leading light in many of the trials of drugs that are currently part of the every physician’s drug armamentarium.
Diamond played a major role in the evolution of the American Association for the Study of Headache and was its chief executive for many years. His autobiography makes it clear that his relationship with the neurological establishment was often fraught. Nevertheless, it is a tribute to his diplomatic skills that the American Headache Society (as it is now called) covers such a broad spectrum of practitioners from neurologists and pediatricians to physiotherapists, psychologists and other colleagues. He also initiated the influential patients’ own National Migraine (now Headache) Foundation.
Rose, in contrast, was more of a neurological polymath, with interests not only in headache but also in motor neurone disease, Parkinson’s disease and stroke. He was perhaps more dependent on his junior colleagues on both the clinical and academic fronts. Diamond’s concentration on one symptom attracted devoted patients from all over the continent. Both were renowned for their approachability.
Diamond’s autobiography was written in conjunction with a medical journalist, in the third person in somewhat more popular style, with many fascinating personal details, including his prowess at Bridge and his innocent dealings with the local mafia. Rose wrote his in the first person, and his voice and characteristic energy come through.
They were both devoted to their wives and children. Diamond and his wife, Elaine, had three girls, of whom one now runs the eponymous Clinic in Chicago after his retirement. Rose and his wife, Angela, had three boys, all established in careers away from medicine.
Both autobiographies give fascinating insights into medical training during and immediately after World War II, as well as into the evolution of the clinical and academic world of headache on each side of the Atlantic. Both are fitting tributes to two outstanding men.
The Headache Godfather: The Story of Dr. Seymour Diamond and How He Revolutionized the Treatment of Headaches By Seymour Diamond and Charlie Morey. Skyhorse Publishing, Inc., New York 2015 ISBN-10: 1629145386 $24.95
Autobiography: By Any Other Name By Clifford Rose Privately printed 2014 [Copies may be available for £12 + p&p. Expressions of interest should be made to r.peatfieldimperial.ac.uk]


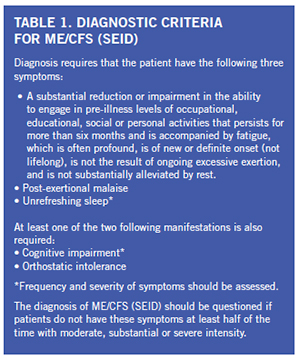 There is significant economic burden associated with this condition as one quarter of patients are bed- or house-bound at some time during their illnesses. ME/CFS patients have been found to be more functionally impaired than patients with other disabling illnesses, such as diabetes mellitus, congestive heart failure, hypertension, depression, multiple sclerosis and end-stage renal disease. Unemployment rates range from 35 to 69 percent in these patients. ME/CFS patients have loss of productivity and high medical costs that lead to an estimated economic burden of $17 billion to $24 billion yearly.
There is significant economic burden associated with this condition as one quarter of patients are bed- or house-bound at some time during their illnesses. ME/CFS patients have been found to be more functionally impaired than patients with other disabling illnesses, such as diabetes mellitus, congestive heart failure, hypertension, depression, multiple sclerosis and end-stage renal disease. Unemployment rates range from 35 to 69 percent in these patients. ME/CFS patients have loss of productivity and high medical costs that lead to an estimated economic burden of $17 billion to $24 billion yearly.