By Chandrashekhar Meshram

Chandrashekhar Meshram
The second wave of the COVID-19 pandemic was devastating in India with a sudden spurt in cases during the second quarter of the year, and with the count of daily cases crossing 400,000. During this pandemic, there was another epidemic of the fungal infection mucormycosis.
This pandemic and epidemic completely exposed the lacunae in the health care system in the country. There was a shortage of medicines, a shortage of hospital beds, a shortage of oxygen supply, and a shortage of health care personnel, resulting in high morbidity and mortality. According to the statement on June 28 by the Union Health Minister, 40,845 cases of mucormycosis were reported in the country. Out of these, 85% patients had COVID-19, 62% had diabetes as a comorbidity, and 63% of patients had received steroids. The alarming fact is that 32% of the patients were in the age group of 18 to 45 years.
Mucormycosis is caused by saprophytic fungi of the order Mucorales, which are found in decaying organic matter and soil samples. Rhizopus Arrhizus is the most common etiological agent in India. Mucormycosis is an angioinvasive disease causing tissue infarction and necrosis. Rhino-orbito-cerebral mucor is the most common presentation, followed by pulmonary, cutaneous, gastrointestinal, renal, and disseminated disease.
Rhino-orbito-cerebral mucormycosis (ROCM) is often encountered by neurologists. Clinical manifestations of ROCM syndrome include new onset unilateral headache, facial pain, facial numbness, orbital pain, diplopia, ophthalmoplegia, impairment of vision, orbital swelling, ptosis, proptosis, papilledema, nasal discharge, and epistaxis. Black discoloration of skin and mucosa are characteristic of mucor infection. Sometimes there is cavernous sinus thrombosis and internal carotid artery block. The majority of patients with ROCM in association with COVID-19 develop symptoms between day 10 and day 15 post COVID-19. However, delayed presentation can occur up to three months.
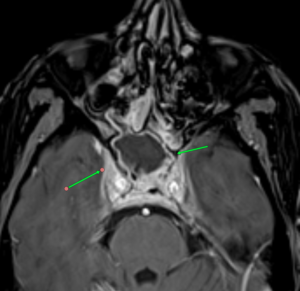
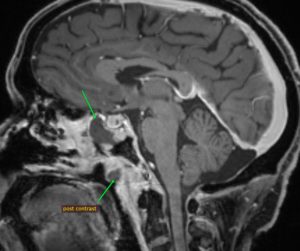
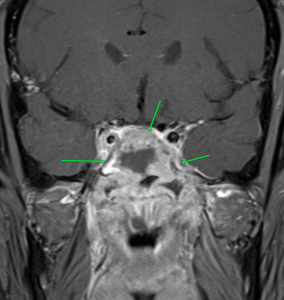 MRI images of mucormycosis with cavernous sinus involvement in a patient with COVID-19.
MRI images of mucormycosis with cavernous sinus involvement in a patient with COVID-19.
Imaging findings on CT or MRI that suggest the diagnosis are non-enhancing hypointense mucosa over nasal turbinate and nasal septum (black turbinate sign), concomitant involvement of paranasal sinuses and orbit, bone erosion or destruction, cavernous sinus involvement (figure), and ischemic stroke.
The diagnosis is confirmed by demonstrating fungus with special stains in tissues obtained from nasal scraping or surgery.
Mucormycosis is a medical emergency, and treatment should start with antifungal drugs, surgical intervention, and correction of metabolic abnormalities or risk factors. Amphotericin B is the first-line drug of choice. Liposomal form of Amphotericin B (LAmpB) is preferred in view of a better side effect profile. The efficacy of conventional deoxycholate amphotericin B (dAmpB) is not inferior to the liposomal form but has more side effects. However, the cost of LAmpB is 10 times more. Nephrotoxicity is the most common side effect of dAmpB.
Other drugs used in the treatment are posaconazole and isavuconazole. Oral medication can be used for longer duration. The duration of treatment is not known and has to be decided on a case-to-case basis. Ampho B is recommended for initial 4-6 weeks, which can be followed by posaconazole or isavuconazole for a few more weeks.
Surgical treatment includes debridement or excision of necrotic tissue. Depending on the site of involvement, an ENT surgeon, ophthalmologist, dental surgeon, and neurosurgeon should be part of the team. Surgical intervention at early stage improves the outcome. Functional endoscopic sinus surgery, paranasal sinus debridement, and orbital exenteration are commonly required surgical procedures in ROCM.
The major drawbacks in managing mucormycosis in India are a gap in treatment protocol and non-affordability of LAmpB due to financial constraints.
The mortality rate of mucormycosis in India is in the range of 28–52%, and it increases to 80% in intracranial extension of disease. High mortality is due to delays in seeking medical attention and diagnosing the disease and challenges in managing the advanced stage of infection. There is an urgent need to increase awareness among the general public and doctors for early diagnosis and treatment.
The intriguing question is why there has been such a recent spurt of cases of mucor in India? Though mucormycosis is globally distributed, its estimated prevalence even before the COVID-19 pandemic was 70 times higher in India as compared to global data. The possible reason for the high prevalence is the abundant presence of Mucorales in the community and the hospital environment and the high prevalence of diabetes in the Indian population. The sudden spurt during the second wave might be due to a lowering of immunity by the new strain of COVID-19 making these patients susceptible for fungal infection. •
Chandrashekhar Meshram is chair of the The Tropical and Geographical Neurology Specialty Group of the WFN.


 The COVID pandemic had universal effects on medicine, and Mumbai was no exception. In fact, being a densely populated city with lots of international travelers, the cases appeared early and the magnitude was high, throwing the health system off gear.
The COVID pandemic had universal effects on medicine, and Mumbai was no exception. In fact, being a densely populated city with lots of international travelers, the cases appeared early and the magnitude was high, throwing the health system off gear.