Meeting promotes ultrasonic techniques and research
By Marina Alpaidze, MD, PhD

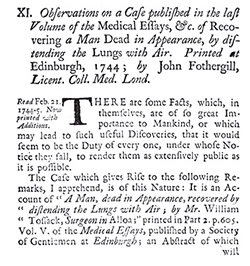
Participants of the second Regional NSRG WFN meeting. From left to right: Marina Alpaidze, MD, President of NSRG WFN Georgian Chapter and President of Georgian Society of Neurosonology and Cerebral Hemodynamics; Alexander Razumovsky, PhD, FAHA, Secretary of NSRG WFN (U.S.); Natan Bornstein, MD, PhD, Vice-President of World Stroke Organization, President of European Society for Neurosonology and Cerebral Hemodynamics (Israel); and Ekaterina Titianova, MD, PhD, Dsc, President of Bulgarian Society of Neurosonology and Cerebral Hemodynamics.
The Neurosonology Research Group (NSRG) WFN is dedicated to the promotion of science and research as well of education and training in the field of ultrasonic techniques and its clinical utilization. Therefore, international cooperation and the dissemination of scientific information within the field of neurosciences and neurosonology is part of NSRG WFN activities.
During Oct. 25-26, 2014, the Georgian Chapter of the NSRG WFN successfully conducted the second NSRG WFN Regional Meeting in Tbilisi, Georgia. There were also participants from neighboring countries — Armenia and Azerbaijan. This two-day course was designed for individuals who are interested to perform and interpret neurosonology studies. The faculty discussed current status of neurosonology and some specific clinical applications; part of the meeting was dedicated to the hands-on practice. The lectures were delivered by well-known neurologists and neurosonology experts such as N. Bornstein (Israel), E. Titianova (Bulgaria), Z. Nadareishvili (U.S.), M. Alpaidze (Georgia), and A. Razumovsky (U.S.).
This second Georgian meeting was guided and directed under the auspices of the NSRG of the WFN and accredited by Tbilisi Medical University Continuing Medical Education (CME) Board for 10 CME hours.



 Stroke is the third leading cause of premature death and disability worldwide. The burden of stroke is growing in low and middle-income countries due to many factors including population growth and aging, urbanization, unhealthy diets, physical inactivity and smoking. More importantly, these demographic and epidemiologic factors are driving a rise in the prevalence of high blood pressure, the leading independent risk factor for both ischemic and hemorrhagic stroke. In many less developed countries, particularly in rural areas, awareness of high blood pressure is extremely low and screening services are non-existent. On the other hand, treatment for high blood pressure is widely available and relatively inexpensive.
Stroke is the third leading cause of premature death and disability worldwide. The burden of stroke is growing in low and middle-income countries due to many factors including population growth and aging, urbanization, unhealthy diets, physical inactivity and smoking. More importantly, these demographic and epidemiologic factors are driving a rise in the prevalence of high blood pressure, the leading independent risk factor for both ischemic and hemorrhagic stroke. In many less developed countries, particularly in rural areas, awareness of high blood pressure is extremely low and screening services are non-existent. On the other hand, treatment for high blood pressure is widely available and relatively inexpensive.
