
Figure 1. Marble bust depicting a young Richard Bright (from Barry and Mackenzie 1998).
Richard Bright was born in 1789 in Bristol. He received his medical training at the University of Edinburgh and at Guys Hospital, which he completed in 1812 with a doctorate on infectious erysipelas. (Berry and Mackenzie).
In 1820, Bright was elected assistant physician to Guy’s Hospital. There, he spent time in the company of a number of physicians whose names like his own became household names in medicine — James Parkinson, Thomas Addison and Thomas Hodgkin.
The eminent surgeon and scholar Sir Astley Cooper encouraged Bright in his research activities and impressed upon him the value of autopsies. After the publication of his epochal studies on diseases of the kidney in 1827, Bright recorded his observations on diseases of the brain. Volume II of his “Reports of Medical Cases” (Bright 1831) contains a wide range of neurological disorders.
The portrait of Bright that accompanies many of his biographical sketches shows him as a somewhat perplexed grandfather. It is likely however, that during his productive period, he resembled more a marble bust of him, which suggests a bright, alert and inquisitive young man. (See Figure 1.)
Bright made seminal observations on diseases of many organs, but it was his work on diseases of the kidneys that earned him undying fame and the title of “The Father of Nephrology.” This monumental accomplishment has overshadowed his important observations on diseases of the brain and other organs.
Apoplexy
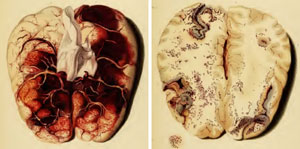
Figure 2. A: Plate V – Thrombosis of the superior sagittal sinus and feeding veins. B: Plate VI – Petechial hemorrhages in cerebral venous thrombosis
Advances in anatomy and physiology initiated in the 16th and 17th centuries and information that accrued from autopsies of apoplectics provided facts that were not reconcilable with the humoral theory. Nevertheless, scholarly physicians at the beginning of the 19th century interested in what was then known as “apoplexy” still faced a bewildering assortment of opinions, dogma and hypotheses. “Apoplexy” was a term used by professionals and the educated laity for a disorder that “struck abruptly, causing a sudden abolition of all the activities of the mind, with the preservation, for a time, of the pulse and respiration” (Bonet).
The rest of the populace used the term “stroke” for this condition. Jean Fernel (1544) and Johann Jacob Wepfer (1658) found intracranial hemorrhage at autopsies of apoplectics. These

Figure 3. Sagittal section though the left hemisphere showing cerebral softening.
observations were repeatedly confirmed, and the notion took hold that apoplexy (stroke) may be a disorder of cerebral blood vessels, rather than an accumulation of phlegm or some other humor in the cerebral ventricles, as proposed by Galen on the basis of the humoral theory.
The classification of apoplexy that emerged from autopsy reports published in the 17th and 18th centuries was still accepted at the beginning of the 19th century: “sanguineous apoplexy,” caused by intracranial hemorrhage, and “serous apoplexy,” in which the effusion of serum was held responsible for the apoplectic state.
Morgagni (1769) recognized a third type of apoplexy, in which neither blood nor serum was effused.
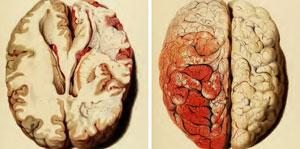
Figure 4. Images from Plates XV and XVI. A: Swelling and softening of the left cerebral hemisphere. B: Striking hyperemia of the swollen hemisphere. The labeling on Plate XV indicates that the right hemisphere was swollen, whereas in Plate XVI the hyperemia is said to be on the left side. It seems that the images are mislabeled.
On the authority of Morgagni and other “great masters,” any amount of fluid present in the ventricles and the subarachnoid space was, for a time, deemed to be abnormal by many scholars and a cause of apoplexy. The concept of “serous apoplexy” endured until the latter part of the 19th century.
Ramolissement
New thoughts on apoplexy emerged as the result of studies at the Paris Hospitals at the turn of the 19th century (Karenberg). While Rochoux (1812) defined apoplexy as cerebral hemorrhage, Rostan’s discovery, published in 1819, of the phenomenon of ramolissement (cerebral softening) in patients with the syndrome of apoplexy, led to new notions concerning this condition. Rostan suggested that ramolissement, was a “disease sui generis,” a primary disease, and that it was peculiar to the brain, while Lallemand (1820) speculated that ramolissement was an inflammatory condition (Karenberg).

Figure 5. Images from Plate IX. Left: Partially clotted aneurysm from a patient with a subarachnoid hemorrhage. (Case CXXV) Right: Arteries of the brain with extensive cerebral atherosclerosis in a patient with intracerebral hemorrhage (case CXXXV).
Bright’s Reports of Medical Cases
Bright held that the ultimate object of medical research was:”to devise remedies most likely to be beneficial in each form of disease,” which, he said, was bound to be facilitated by the understanding of their causes.
To this end, he arranged his cases of diseases of the brain into sections according to what were then understood to be “…. the more obvious sources of disease,” namely inflammation, pressure, irritation and inanition.
This article provides a review of Bright’s observations and thoughts on apoplexy or stroke, which he recorded in the sections on inflammation and pressure.
Inflammation and Cerebral Softening
In the section on inflammation, Bright described cases illustrative of various inflammatory disorders, such as meningitis, intracranial suppuration, as well as cerebral congestion and also deficient cerebral circulation.
With the first case in this group, Bright established that cerebral softening may be caused by cerebral congestion due to cerebral venous thrombosis. (See Figure 2.) He concluded that venous thrombosis occurred in debilitated states, which in his patient he attributed to pneumonia. To illustrate “the tendency to coagulate which the blood acquires when the system is under the influence of different debilitating causes,” he added three cases with systemic venous thrombosis associated with chronic illness and one with ovarian cancer.
Ramolissement Due to Deficient Blood Supply
In the last five cases in this section, cerebral softening was presented as the principal pathological finding. Bright stated that the symptoms generated by cerebral softening resemble those caused by “pressure,” which he believed to be the ultimate source of the cardinal symptoms of apoplexy, namely paralysis and impaired consciousness.
Case LXXXI was a 68-year-old man who suddenly became unconscious. When he regained consciousness after 10 minutes, he was hemiplegic on the right, with right hemisensory loss and aphasia. Death occurred about three weeks after the onset of his illness. Softening of the anterior part of the left cerebral hemisphere extending from the fossa Sylvii to the corpus striatum was discovered at autopsy. (See Figure 3.) (Case LXXXI, p 178). The arteries of “fossa Sylvii” “fossa Sylvii,” the carotids and of the circle of Willis were extensively diseased, the mitral valve was abnormal.
In the next two cases, the illness developed gradually, and the patients were young (28 and 30 years). Autopsy showed extensive cerebral softening. In one of these cases, there was a remarkable cortical hyperemia of the swollen and softened cerebral hemisphere. (See Figure 4.)
These cases showed severe ossification of the arteries and extensive cerebral softening of one cerebral hemisphere. Bright stated that abnormal arteries: “… certainly produced in my mind an impression that the proper supply of blood had been cut off by some change in the vessels of the pia mater, or some obstruction in their passage through the cineritious substance, and in this way death and disorganization of the brain had been produced.”
Bright stated that “ossification of the arteries might well be considered as laying the foundation for defective circulation,” and that cerebral softening corresponded to gangrene of the limbs.
These three cases constitute the basis for a concept that was novel at that time, namely that apoplexy (stroke) may be caused by arterial obstruction as well as by the extravasation of blood.
Cases Illustrating the Effects of Pressure
The section on the effects of “pressure” includes cases illustrative of the effects of vascular turgescence, “pressure of the brain from serous effusion independent of inflammation,” cases in which some organic change had given rise to pressure, and cases in which blood had been effused from ruptured vessels.
Bright’s attempts at localization, which he believed was of importance for accurate diagnosis, represents a significant advance toward modern neurology.
Pressure Due to Effused Serum
Bright maintained that by generating pressure effused serum caused or enhanced apoplexy. He did not use the term “serous apoplexy,” but his cases “illustrating the occurrence of pressure of the brain from serous effusion independent of inflammation” show that he could not free himself of the concept of “serous apoplexy.”
Pressure Due to Extravasation of Blood
The subsection on intracranial hemorrhage begins with five cases “in which the effusion of blood has been found upon the surface of the brain.” Here Bright gives excellent descriptions of the symptoms that characterize subarachnoid hemorrhage.
In one of these cases, a 19-year-old man “while sitting on the chamber utensil suddenly exclaimed, ‘Oh my head.'” Bright found blood on the surface of the brain and a ruptured, partially clotted middle cerebral artery aneurysm. (See Figure 5a.)
The remainder of the cases in this section showed intracranial hematomas of various ages and a subdural hematoma. The arteries showed evidence of atherosclerosis (See Figure 5b), not only in older patients, but also in young apoplectics.
Bright noted severe bradycardia in a patient with a subdural hematoma and suggested that “it is by no means improbable that the pressure experienced by the brain during the existence of the coagulum…had some share in producing the retarded circulation.”
A patient who suffered “successive paralytic attacks” and eventually reached a “state of imbecility” showed multiple small softenings of the brain at autopsy, “the brain resembling ‘Parmasan’ ” (sic) cheese.” The aortic and mitral valves were “very much thickened.” Bright declared that the size of the softenings was related to the size of the diseased vessel.
In this description, we recognize TIAs (transient ischemic attacks), RINDs (reversible ischemic neurologic deficits), vascular dementia and lacunes.
Additional symptoms preceding apoplexy recorded by Bright were: headache, giddiness, migraine-like headaches, numbness left face, two or three attacks of hemiplegia, successive slight attacks of transient hemiplegia, affecting sensation more than motion, occasional vertigo and episodic incoherence.
Bright maintained that the location of disease in the brain or the blood vessels determined the nature of the symptoms. He furthermore suggested that the awareness of this fact would enhance diagnostic accuracy, which in turn was bound to improve treatment.
Unusual Cases
Bright recorded two unusual cases: Hemiplegia ipsilateral to the cerebral lesion and “tormenting pain” in paralyzed limbs that were deprived of sensation.
He was skeptical about the genuineness of signs ipsilateral to the brain lesion: “having once or twice nearly deceived myself by the imperfect accounts of friends in such cases, I am not willing to admit them hastily.”
Treatment of Apoplexy
“It is impossible to remove a strong attack of apoplexy and not easy to remove a weak attack.” (Hippocrates)
This Hippocratic aphorism did not deter physicians from trying to cure apoplexy, both strong and weak.
Although it was well known that some apoplectics survived without any treatment. Survival was usually credited to treatment, and it was often implied that death resulted when treatment was inadequate or withheld. This helped to perpetuate the belief in the effectiveness of the diverse interventions then in fashion.
“In the treatment of apoplexy, the most important point is the employment of bleeding; the judicious use of which powerful remedy the cure greatly depends.” (Bright 1831, p 334)
Although the methods of treatment in the early 19th century were still based largely on surviving humoral concepts, Bright’s rationale for abstracting blood was “a view of checking the hemorrhage,” and the hope of reducing congestion rather than the restoration of a balance of the four humors. The supplemental maneuvers had the same rationale for Bright.
Whatever the rationale, the abstraction of blood was the recommended remedy for apoplexy and a nearly universal practice in Bright’s time. Venesection or arterial section close to exsanguination, supplemented by the application of leeches, cupping, both wet and dry, were standard procedures in the treatment of apoplexy and for many other ailments. The pulse was monitored and abstraction was stopped when the pulse became depressed. Caution was advocated in the exsanguination of feeble individuals. The energetic bleeding that was practiced at that time must have lowered blood pressure for a time, and therefore might have reduced bleeding.
Blisters and Setons were used as additional supplements to bleeding. Purging was in regular use. The induction of vomiting was occasionally practiced but it was considered harmful by those who feared that the strain associated with vomiting may be harmful.
Bright used stimulants when “the patient grew cold” and “the pulse fluttering.” He poured “vinegar down the throat, brandy if it could be procured” or “a few drops of compound spirits of ammonia to elicit cough that tended to rouse the patient.” Cloth dipped in hot water was applied to the stomach. Cold cloths were “dashed on the temples and forehead with a sudden jerk,” when the head felt hot and the carotids were throbbing. Frequently, the head was shaved, and cold applied to the shaven head.
Such therapy persisted throughout the 19th century, and bloodletting for stroke was not unknown in the 20th century. Few went as far as Thomas Sydenham, who stated: “I have consulted my patients’ safety and my own reputation most effectually by doing nothing at all.”
Summary
Bright showed that cerebral softening has many causes, one of which was a deficient blood supply caused by diseased arteries which like Abercrombie (p.25), he considered to be analogous to the gangrene of limbs.
Bright has shown that cerebral softening can be caused by thrombosis in the cerebral venous system. He also suggested that chronic illness and malignancy are risk factors for venous thrombosis. Bright also believed that venous obstruction contributed to thrombosis in his case of ovarian cancer. He thus came close to anticipating Virchow’s coagulation triad (stasis, abnormal blood, diseased blood vessels).
The determination by Bright that cerebral softening was caused by a deficiency of blood supply represents a significant advance in the understanding of cerebrovascular disease.
Bright’s description of the symptomatology of subarachnoid hemorrhages compares well with current accounts. His demonstration of a partially clotted aneurysm as a cause of an intracranial hemorrhage was one of the earliest observations of its kind.
Bright described TIAs and reversible ischemic neurological deficits (RINDs), and the lacunes that may result from them, and he recognized that dementia may be caused by multiple areas of cerebral ischemia. He further recognized that small lacunes were the result of obstructions of small arterial branches, whereas the obstruction of larger branches caused larger cavities. Although the realization that these were embolic came later, he did document carotid and valvular disease in a number of cases.
Bright associated bradycardia with intracranial hypertension.
He also gave a good description of intractable pain in pain paretic limbs with “destroyed sensation,” now known as “the thalamic syndrome of Déjérine.” He mentioned a case of paralysis ipsilateral to a cerebral lesion, but was hesitant to accept it as genuine.
Bright’s attempts at localization, which he believed was of importance for accurate diagnosis, represents a significant advance toward modern neurology.
Richard Bright’s observations on cerebral softening and apoplexy contributed to the current understanding of cerebrovascular disease and its division into occlusive and hemorrhagic strokes.
References
1. Abercrombie, J. Pathological and practical researches on diseases of the brain and the spinal cord. Edinburgh, Waugh and Innes.1828.
2. Berry, D, Mackenzie C. Richard Bright 1789-1858. Physician in an Age of Revolution and Reform. Royal Society of Medicine Services, Ltd. 1992.
3. Bright, R. Reports of medical cases selected with the view of illustrating the symptoms and cure of diseases. Vol I, Vol II London, Longman.1827, 1831.
4. Fernel, J. Universa Medicina. Geneva. De Tornes. 1544.
5. Karenberg, A. Stroke at the Paris Hospitals. The emergence of anatomico-clinical concepts after 1810. J. Hist. Neurosc. 19: 390.1872. 2010
6. Lallemand F.Researches anatomo-pathologiques sur l’encéphale et ses dépendences. Paris. 1820
7. Morgagni, GB. The Seats and Causes of Disease, Vol. 1, London, McMillan and Cadell, 1769.
8. Rochoux, J A, Recherches sur L’Apoplexie, Paris, Bechel Jeune. 1814.
9. Rostan, L.. Recherches sur le ramollissement du cerveau; ouvrage dans lequel on s’efforce de distinguer les diverses affections de ce viscè
re par des signes caractéristiques. 2nd Edition, Paris, Bechet. 1819.
10. Schutta, HS, Abu-Amero, KK, Bosley, TM. Exceptions to the Valsalva doctrine. Neurology, 74: 329-335. 2010.
11. Wepfer, J. J. Observationes anatomical, ex cadaveribus eorum quo sustulit apoplexia, cum exercitation ejus loco affecto. Schaffhausen, 1658.
