The legacy of this Alzheimer’s researcher was to live life as it came.
By Natalia Acosta-Baena, AND Ricardo Nitrini
 Francisco Javier Lopera Restrepo passed away on Sept. 10, 2024, a great loss for his family, friends, collaborators, for all of science, and for neurosciences in Latin America. He leaves the advances brought by his studies as well as a great legacy that includes important developments and a large number of high-quality disciples.
Francisco Javier Lopera Restrepo passed away on Sept. 10, 2024, a great loss for his family, friends, collaborators, for all of science, and for neurosciences in Latin America. He leaves the advances brought by his studies as well as a great legacy that includes important developments and a large number of high-quality disciples.
Dr. Lopera was born on June 10, 1951, in Aragón, a small town in Santa Rosa de Osos, a municipality of Antioquia, Colombia. He came from a rural family with strong roots. His parents taught him everything he practiced. From his mother, he got his drive and humility. From his father, his love for knowledge. One anecdote he shared recalled when his father bought all his children a Larousse dictionary and exclaimed: “The summary of knowledge.” His mother sewed shorts from sackcloth for each of her 13 children. She also always knew how to make sure they were well. When Dr. Lopera got married, the bride’s father told her: “Remember that you are also marrying science.” And so it was. His life was neuroscience.
After receiving the title of neurologist, when he left Colombia in 1987 to complete his neuropsychology training at the Catholic University of Louvain, Belgium, he carried under his arm the genealogies of the families with early Alzheimer’s that he had identified and described while he was a neurology resident.1 But nobody paid attention to him.
He returned to Colombia in 1989 and served as coordinator of the Neurosciences Group of the University of Antioquia (GNA). It was not until 1995 that a mutation (E280A) was found in the presenilin 1 gene, in collaboration with Kenneth Kosik and Alison Goate.2 A longitudinal follow-up was carried out on all subjects identified to date, and 15 years later, a description was made of the natural evolution of the disease in this population, identifying the ages of onset for the preclinical and clinical stages.3
This study was the only one carried out solely by Colombian researchers. It was crucial for the design of the clinical trial with crenezumab that came later, and it was the basis for determining the ages of the cohort and detecting protective genes. The beginning of gains and strength in research in Colombia and Latin America arrived in the 2000s.
Alzheimer’s Research
Much will be written about the importance of Dr. Lopera for advancing knowledge about Alzheimer’s disease, but there are some aspects that may be considered more important for the entire research community, especially for those from low- and middle-income countries.
Most of Dr. Lopera’s publications are about autosomal dominant Alzheimer’s disease caused by the E280A mutation of the presenilin 1 gene. From his careful studies of this kindred, he was able to obtain enough data to transform it into the world’s largest autosomal dominant Alzheimer’s disease kindred, which contributed to the knowledge of several steps in the evolution of Alzheimer’s disease.
There were two groups of studies that came from Dr. Lopera’s research. The first group made it possible to verify the first changes in biomarkers, the time interval between these changes and the first symptoms hallmarking the onset of dementia. These discoveries revealed that the interval between changes in biomarkers and dementia is greater than 20 years.3,4
The second group is related to the case of a patient named Aliria who, having the E280A mutation of presenilin 1, did not develop mild cognitive impairment until her 70s, three decades after the expected age of clinical onset.3,5 Aliria died at the age of 77 without dementia; the average age at which dementia occurs in the disease caused by this mutation is about 49 years.5,6
The neuropathological examination confirmed the presence of unusually high brain amyloid levels and limited tau and neurodegenerative measurements,6 which had already been revealed by amyloid and tau PETs performed years before.5 The patient had two copies of the APOE3 Christchurch (R136S) mutation, which points to the role of apolipoprotein E (APOE) in the pathogenesis, treatment, and prevention of Alzheimer’s disease.5,6
Lifetime Achievements
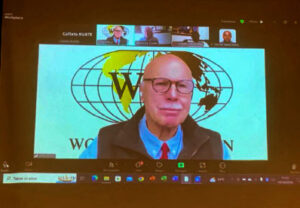
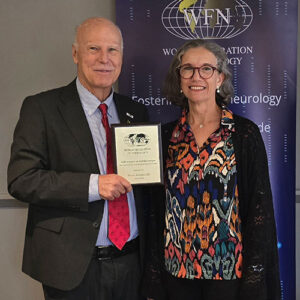
These and many other contributions made by Dr. Lopera were rightly awarded, most notably the Bengt Winblad Lifetime Achievement Award, presented by the Alzheimer’s Association in 2020, and the Potamkin Prize (often called the “Nobel Prize of Alzheimer’s Research”) from the American Academy of Neurology (AAN) and the American Brain Foundation (ABF) in 2024.
In addition to the importance of these studies for scientific knowledge, there is much to be learned from them by all researchers in Latin America.
First, Dr. Lopera demonstrated tenacity, persistence, focus, and the firm conviction that this work would lead to additional important discoveries. Between the first publication on this autosomal dominant Alzheimer’s disease and the Aliria case, 32 years of continued studies passed.1,5
Second, but no less important, Dr. Lopera had good collaborators among his colleagues and students. He also chose the best international collaborators who did not look at a researcher from a low- and middle-income country as a mere data provider to enrich their own research. Even though he would not have achieved this depth of research without international collaboration, Dr. Lopera always remained the main researcher and unquestionable leader of his publications.
Like many neurologists of his time, Dr. Lopera began studying dementia through studies in neuropsychology, as can be seen from some articles on these topics among his first publications.7,8 During his career, he also kept an in-depth knowledge of cognitive and behavioral neurology.
Another highlight of Dr. Lopera’s career is the research with social commitment that he sought to develop. For example, he conducted field work to evaluate patients with a social plan, where the genetic risk of the disease was disclosed along with the possibility of monitoring and accompanying the sick. Researching patients and helping to improve their quality of life at the same time was somewhat revolutionary. Maintaining a balance between consent without falling into coercion continues to be a significant challenge in vulnerable populations.
Face of Hope
The social plan was consolidated to improve the living conditions of the sick and their caregivers with money from some projects. Support groups, dance, painting, rehabilitation, and mental health were included in the course of the Global Neurology Academy (GNA) learning process. Diapers and wheelchairs were more useful to people than any medication. Unfortunately, it is still the same. And that is why Dr. Lopera used the social plan when starting any clinical trial in these families. Every year, GNA celebrated Christmas with all of the research participants.
Dr. Lopera defended the idea that if one day a medicine tested on this population proves effective, the families of Colombia should be compensated. The thousands of patients in Colombia saw in him the face of hope. They remind us of a worldwide desire: a life-changing medicine that can also be distributed with equity and justice.
Dr. Lopera was a joyful person. He enjoyed food, music, dancing, and everything that life gave him. “Live life as it comes” was one of his last thoughts. Words consistent with his medical practice when speaking to the patients who need to be reminded that they can live with Alzheimer’s. •
Natalia Acosta-Baena is a researcher with Grupo de Neurociencias de Antioquia (GNA), Facultad de Medicina at the Universidad de Antioquia, Colombia. Ricardo Nitrini is a senior professor of neurology with Grupo de Neurologia Cognitiva e do Comportamento (GNCC), Faculdade de Medicina da Universidade de São Paulo, Brazil.
References:
1. Cornejo, W., Lopera, F., Uribe, C. S., & Salinas, M. (1987). Descripción de una familia con demencia presenil tipo Alzheimer. Acta Médica Colombiana, 12(2), 55-61. https://www.actamedicacolombiana.com/ojs/index.php/actamed/article/view/3695.
2. Alzheimer’s Disease Collaborative Group. The structure of the presenilin 1 (S182) gene and identification of six novel mutations in early onset AD families. Nat Genet. 1995 Oct;11(2):219-22. doi: 10.1038/ng1095-219. PMID: 7550356.
3. Acosta-Baena N, Sepulveda-Falla D, Lopera-Gómez CM, Jaramillo-Elorza MC, Moreno S, Aguirre-Acevedo DC, Saldarriaga A, Lopera F. Pre-dementia clinical stages in presenilin 1 E280A familial early-onset Alzheimer’s disease: a retrospective cohort study. Lancet Neurol. 2011 Mar;10(3):213-20. doi: 10.1016/S1474-4422(10)70323-9. Epub 2011 Feb 4. PMID: 21296022.
4. Reiman EM, Quiroz YT, Fleisher AS, Chen K, Velez-Pardo C, Jimenez-Del-Rio M, Fagan AM, Shah AR, Alvarez S, Arbelaez A, Giraldo M, Acosta-Baena N, Sperling RA, Dickerson B, Stern CE, Tirado V, Munoz C, Reiman RA, Huentelman MJ, Alexander GE, Langbaum JB, Kosik KS, Tariot PN, Lopera F. Brain imaging and fluid biomarker analysis in young adults at genetic risk for autosomal dominant Alzheimer’s disease in the presenilin 1 E280A kindred: a case-control study. Lancet Neurol. 2012 Dec;11(12):1048-56. doi: 10.1016/S1474-4422(12)70228-4. Epub 2012 Nov 6. PMID: 23137948; PMCID: PMC4181671.
5. Arboleda-Velasquez JF, Lopera F, O’Hare M, Delgado-Tirado S, Marino C, Chmielewska N, Saez-Torres KL, Amarnani D, Schultz AP, Sperling RA, Leyton-Cifuentes D, Chen K, Baena A, Aguillon D, Rios-Romenets S, Giraldo M, Guzmán-Vélez E, Norton DJ, Pardilla-Delgado E, Artola A, Sanchez JS, Acosta-Uribe J, Lalli M, Kosik KS, Huentelman MJ, Zetterberg H, Blennow K, Reiman RA, Luo J, Chen Y, Thiyyagura P, Su Y, Jun GR, Naymik M, Gai X, Bootwalla M, Ji J, Shen L, Miller JB, Kim LA, Tariot PN, Johnson KA, Reiman EM, Quiroz YT. Resistance to autosomal dominant Alzheimer’s disease in an APOE3 Christchurch homozygote: a case report. Nat Med. 2019 Nov;25(11):1680-1683. doi: 10.1038/s41591-019-0611-3. Epub 2019 Nov 4. PMID: 31686034; PMCID: PMC6898984.
6. Sepulveda-Falla D, Sanchez JS, Almeida MC, Boassa D, Acosta-Uribe J, Vila-Castelar C, Ramirez-Gomez L, Baena A, Aguillon D, Villalba-Moreno ND, Littau JL, Villegas A, Beach TG, White CL 3rd, Ellisman M, Krasemann S, Glatzel M, Johnson KA, Sperling RA, Reiman EM, Arboleda-Velasquez JF, Kosik KS, Lopera F, Quiroz YT. Distinct tau neuropathology and cellular profiles of an APOE3 Christchurch homozygote protected against autosomal dominant Alzheimer’s dementia. Acta Neuropathol. 2022 Sep;144(3):589-601. doi: 10.1007/s00401-022-02467-8. Epub 2022 Jul 15. PMID: 35838824; PMCID: PMC9381462.
7. Lopera F. Procesamiento de caras: bases neurológicas, trastornos y evaluación [Procesing of faces: neurological bases, disorders and evaluation]. Rev Neurol. 2000 Mar 1-15;30(5):486-90. Spanish. PMID: 10775980.
8. Sierra M, Lopera F, Lambert MV, Phillips ML, David AS. Separating depersonalisation and derealisation: the relevance of the “lesion method.” J Neurol Neurosurg Psychiatry. 2002 Apr;72(4):530-2. doi: 10.1136/jnnp.72.4.530. PMID: 11909918; PMCID: PMC1737835.