 By Scott E. Kasner, MD, and Ralph L. Sacco, MD
By Scott E. Kasner, MD, and Ralph L. Sacco, MD
Note: The views expressed by the authors are their own and do not represent an official statement by the American Heart Association/American Stroke Association.
Stroke was defined by the World Health Organization (WHO) more than 40 years ago as “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than that of vascular origin.”1 This was a working definition created for a study assessing the prevalence and natural history of stroke, and it served its purpose at the time.
The ensuing decades have witnessed major advances in basic science, pathophysiology and neuroimaging that have dramatically improved our understanding of ischemia, infarction and hemorrhage in the central nervous system (CNS). There is little doubt that permanent injury occurs well before the 24-hour threshold, and therefore purely time-based definitions are inaccurate and obsolete. Further, neuroimaging has demonstrated that clinically transient symptoms are often associated with evidence of acute cerebral infarction and that infarction may occur without overt symptoms.
In 2009, the American Heart Association/American Stroke Association (AHA/ASA) published a scientific statement redefining transient ischemic attack (TIA) as, “a transient episode of neurological dysfunction caused by focal brain, spinal cord or retinal ischemia without acute infarction.”2 This statement formally addressed only one side of the proverbial coin, but clearly implied that objective evidence of infarction should be considered as a defining feature of stroke.
In the spring of 2013, the AHA/ASA published an expert consensus document with a new definition of stroke to reflect these advances.3 Authors with expertise in the fields of neurology, neurosurgery, neuroradiology, neuropathology, clinical research methods, epidemiology, biomarkers, policy and global public health were invited from within the AHA/ASA, as well as the American Academy of Neurology, the American Association of Neurological Surgeons and Congress of Neurological Surgeons, U.S. Centers for Disease Control and Prevention, the National Institute of Neurological Disorders and Stroke, the European Stroke Organization (ESO), the World Stroke Organization (WSO) and others to establish a universal definition of stroke.
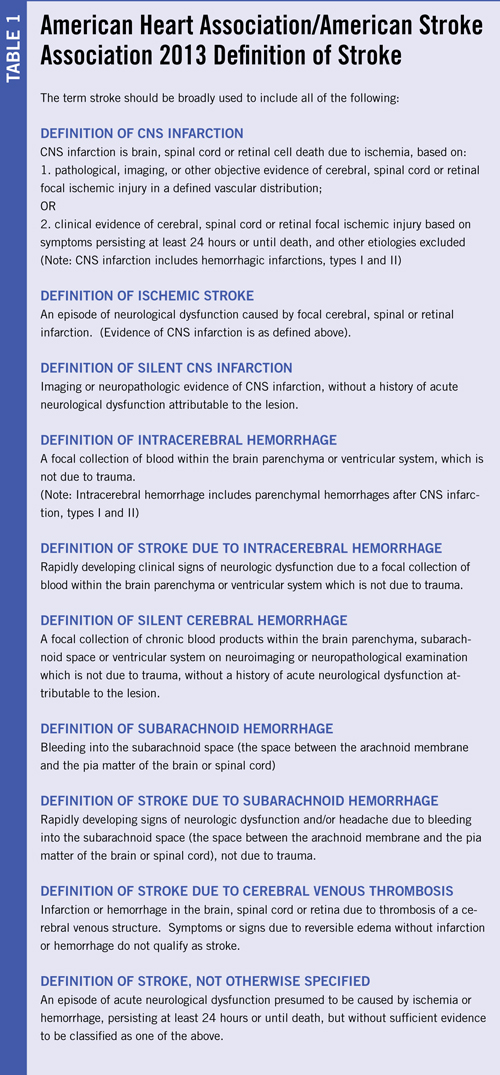
The key components of the new AHA/ASA definition are summarized in Table 1. The major fundamental change compared with older definitions is that the new broader definition of stroke includes any objective evidence of permanent brain, spinal cord or retinal cell death due to a vascular cause based upon pathological or imaging evidence with or without the presence of clinical symptoms. The new definition harmonizes with our understanding of the pathophysiology of infarction and with the recent redefinition of TIA, but also necessitates the inclusion of silent infarction and silent hemorrhage within the broad definition of stroke. Ultimately, the leaders of the ESO and WSO withdrew from participation and declined to endorse the statement because they disagreed about the inclusion of silent cerebral infarction and silent cerebral hemorrhage within the lexicon of stroke. (See “Stroke Definition in the ICD-11 at the WHO.“)
Objective Evidence of CNS Infarction: Imaging or Persistent Symptoms
The AHA/ASA defined CNS infarction based on pathological, imaging or other objective evidence of infarction. In the absence of this evidence, the persistence of symptoms of at least 24 hours or until death remained a method to define stroke. Objective evidence of infarction is generally currently available in the form of neuroimaging or less commonly neuropathological examination, but other methods such as highly sensitive and specific biomarkers may emerge in the future.
At present, imaging is not always available and also is not perfect. CT is well known to have limited sensitivity to acute infarction, especially in the first few hours, and also misses small infarctions even at later time points. MRI is far more sensitive, potentially within minutes of onset, but still fails for small infarctions, especially in the brainstem. In much of the developing world and in rural parts of more developed regions, neither of these tools may be available in the acute setting, if at all, which limits the global applicability of an imaging-based definition of stroke.
Persistence of clinical symptoms also can be taken as objective evidence of cerebral infarction. Several studies suggest that the majority of transient stroke symptoms resolve in less than 24 hours,4,5 and that persistence beyond 24 hours is almost always associated with MRI evidence of infarction. These findings support the classic threshold as a means to infer infarction when there is no confirmatory method readily available.
Definitions and Implications of Silent CNS Infarctions and Hemorrhages
CNS infarction included ischemic stroke, as well as silent CNS infarction (carefully worded to deliberately not use the term “silent stroke”). Ischemic stroke was defined as an episode of neurological dysfunction (clinical symptoms) caused by focal cerebral, spinal, or retinal infarction, while silent CNS infarction was defined as imaging or neuropathologic evidence of CNS infarction, without a history of acute neurological dysfunction attributable to the lesion. Similar definitions were crafted for cerebral hemorrhage. This major departure from past definitions is based on the observation of brain injury, either by imaging or pathological assessment, in patients without a history of well-defined neurologic symptoms.
Silent lesions have been recognized pathologically as infarctions and hemorrhages since the 1960s but were deemed of uncertain importance. However, they may not be entirely asymptomatic, as patients may have subtle cognitive, gait or other functional impairments in the absence of a typical acute presentation. To some extent, the “silence” of an infarction or hemorrhage depends on the eye of the beholder. Patients may not be aware of their symptoms due to neglect, denial or simply may attribute them to another cause and not seek a medical opinion. Physicians and other health care providers may vary in their ability to detect mild neurologic abnormalities, or they, too, may ascribe them to an alternative cause.
Silent CNS infarcts are well-recognized to be associated with impaired mobility, physical decline, depression, cognitive dysfunction, dementia and clinical stroke. Silent brain infarcts increase the risk of ischemic stroke by 2-4 times6,7 independent of other vascular and stroke risk factors. A recent review of MRI diagnostic criteria for silent brain infarcts found a threshold size of ≥3 mm to be a reliable indicator of these lesions. Silent infarcts are approximately 5 times more prevalent than ischemic strokes, found in 8 to 28 percent of patients, and are increasingly prevalent with age and in women.8-13 Chronic small parenchymal hemorrhages, or “microbleeds,” are found in up to 6 percent of healthy elderly individuals.14 These lesions, typically observed on gradient echo sequences on MRI, are the detritus of prior hemorrhages in the form of hemosiderin, typically adjacent to small blood vessels. Microbleeds appear to share the same underlying pathophysiology as larger hemorrhages, and are most commonly associated with cerebral amyloid angiopathy (CAA) and/or chronic hypertension. Since hemorrhage in the brain is always abnormal, there is no size threshold for microbleeds, unlike small infarctions. These microbleeds may not be associated with a clinical event but are associated with cognitive decline”‘5,16 as well as a high rate of subsequent ICH and ischemic stroke.17 As with silent CNS infarctions, the clinical impact may depend on the sensitivity of the observer.
The AHA/ASA included silent CNS infarctions and hemorrhages within the broadest definition of stroke for multiple reasons. First and foremost, since silent lesions have the same pathophysiology as clinically apparent ischemic and hemorrhagic strokes, it seems consistent that they should be united within the same broad disease category. Similarly, the multi-organization Universal Definition of Myocardial Infarction (MI),18 considered any pathologically defined cardiac infarction as an MI, regardless of the presence or absence of any symptoms or signs. Further, inclusion of silent CNS infarction and hemorrhage raises awareness of the potential for cognitive and functional decline that must be assessed and addressed from the perspectives of treatment and prevention. It seems clear that CNS infarctions and hemorrhages occur over a spectrum ranging from severe symptoms to very mild or even clinical silence, and the opinion of the AHA/ASA was that all must be included within the new and broader definition of stroke.
Implications for World Neurology
The new tissue-based definition of CNS infarction depends on either early objective (currently neuroimaging) evidence of infarction or persistence of symptoms for at least 24 hours. If early imaging is not available, then clinicians are left with a diagnostic dilemma in those first 24 hours since the event cannot be clearly classified as stroke. For patients with acute myocardial ischemia, the term “acute coronary syndrome” (ACS) is used before it can be determined if there is infarction or not, as assessed by electrocardiography or biomarkers. Similarly with stroke, the term “acute cerebrovascular syndrome” (ACVS) would suggest the potential diagnoses of cerebral infarction, TIA, and hemorrhage in patients presenting within the first 24 hours from onset and prior to the completion of imaging studies. Ultimately, diagnostic techniques and/or time will help define infarct or hemorrhage based on objective imaging, or TIA in the absence of positive imaging and resolution of symptoms within 24 hours from onset. A major challenge for the future will be the achievement of access to diagnostic and treatment tools in the developing world, where a substantial portion of the global burden of stroke occurs.
The inclusion of silent infarcts and microhemorrhages within the AHA/ASA definition of stroke opens many questions for clinicians. In regions with little or no access to neuroimaging, this change in definition may prove irrelevant for many years to come. However, for those with such access, silent lesions are likely to be detected as a result of the widespread use of MRI for non-cerebrovascular symptoms such as headache or dizziness. Further, clinicians and patients should be aware of the relationship between silent infarcts and hemorrhages with dementia and other impairments. The clinician should consider such patients as having evidence of cerebrovascular disease and should evaluate and treat any potential stroke risk factors. However, guidelines for secondary stroke prevention19 have been generated from clinical trials that have only included patients with symptomatic cerebrovascular disease and have not included silent infarcts. No studies have yet addressed the safety and efficacy of secondary prevention measures in patients who only have silent infarction. Future guidelines must address the available evidence for treatment in this population.
Updating the definition of disease can have prominent effects on disease surveillance and assessments of public health. In the case of adding a large number of silent infarction cases to the existing number of stroke cases, this will increase the total number of stroke cases while likely decreasing the mortality rate due to the addition of a number of minor/silent cases.20 Updating the definition of stroke could result in reclassification of stroke cases for incidence, prevalence, and mortality in national and international statistics, disease classification coding systems and existing health surveys. This is particularly problematic if definitions are applied differently in each region of the globe, and this is a major concern of all stroke organizations. Therefore, the AHA/ASA recommended that symptomatic and silent infarctions and hemorrhages should be counted separately to allow for valid analyses of temporal and geographic trends in stroke. Although the WSO, ESO and WHO will not include the silent lesions within the definition of stroke, they recognize their importance and are going to start counting them within the scope of cerebrovascular disorders in the ICD-11.
Kasner is with the University of Pennsylvania and Sacco is with the University of Miami.
References:
1. Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980;58:113-130.
2. Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, Hatsukami TS, Higashida RT, Johnston SC, Kidwell CS, Lutsep HL, Miller E, Sacco RL. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276-2293.
3. Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, Higashida RT, Hoh BL, Janis LS, Kase CS, Kleindorfer DO, Lee JM, Moseley ME, Peterson ED, Turan TN, Valderrama AL, Vinters HV. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064-2089.
4. Levy DE. How transient are transient ischemic attacks? Neurology. 1988;38:674-677.
5. Shah SH, Saver JL, Kidwell CS, Albers GW, Rothwell PM, Ay H, Koroshetz WJ, Inatomi Y, Uchino M, Demchuk AM, Coutts SB, Purroy F, Alvarez-Sabin JS, Sander D, Sander K, Restrepo L, Wityk RJ, Marx JJ, Easton JD. A multicenter pooled, patient-level data analysis of diffusion-weighted MRI in TIA patients. Stroke. 2007;38:463.
6. Bernick C, Kuller L, Dulberg C, Longstreth WT, Jr., Manolio T, Beauchamp N, Price T. Silent MRI infarcts and the risk of future stroke: the cardiovascular health study. Neurology. 2001;57:1222-1229.
7. Vermeer SE, Hollander M, van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MM. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke. 2003;34:1126-1129.
8. Howard G, Wagenknecht LE, Cai J, Cooper L, Kraut MA, Toole JF. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke. 1998;29:913-917.
9. Kohara K, Fujisawa M, Ando F, Tabara Y, Niino N, Miki T, Shimokata H. MTHFR gene polymorphism as a risk factor for silent brain infarcts and white matter lesions in the Japanese general population: The NILS-LSA Study. Stroke. 2003;34:1130-1135.
10. Longstreth WT, Jr., Bernick C, Manolio TA, Bryan N, Jungreis CA, Price TR. Lacunar infarcts defined by magnetic resonance imaging of 3660 elderly people: the Cardiovascular Health Study. Arch Neurol. 1998;55:1217-1225.
11. Price TR, Manolio TA, Kronmal RA, Kittner SJ, Yue NC, Robbins J, Anton-Culver H, O’Leary DH. Silent brain infarction on magnetic resonance imaging and neurological abnormalities in community-dwelling older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. Stroke. 1997;28:1158-1164.
12. Vermeer SE, Koudstaal PJ, Oudkerk M, Hofman A, Breteler MM. Prevalence and risk factors of silent brain infarcts in the population-based Rotterdam Scan Study. Stroke. 2002;33:21-25.
13. Vermeer SE, Longstreth WT, Jr., Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611-619.
14. Roob G, Schmidt R, Kapeller P, Lechner A, Hartung HP, Fazekas F. MRI evidence of past cerebral microbleeds in a healthy elderly population. Neurology. 1999;52:991-994.
15. Qiu C, Cotch MF, Sigurdsson S, Jonsson PV, Jonsdottir MK, Sveinbjrnsdottir S, Eiriksdottir G, Klein R, Harris TB, van Buchem MA, Gudnason V, Launer LJ. Cerebral microbleeds, retinopathy, and dementia: the AGES-Reykjavik Study. Neurology. 2010;75:2221-2228.
16. Werring DJ, Frazer DW, Coward LJ, Losseff NA, Watt H, Cipolotti L, Brown MM, Jager HR. Cognitive dysfunction in patients with cerebral microbleeds on T2*-weighted gradient-echo MRI. Brain. 2004;127:2265-2275.
17. Fan YH, Zhang L, Lam WW, Mok VC, Wong KS. Cerebral microbleeds as a risk factor for subsequent intracerebral hemorrhages among patients with acute ischemic stroke. Stroke. 2003;34:2459-2462.
18. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third Universal Definition of Myocardial Infarction. Circulation. 2012.
19. Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, Halperin JL, Johnston SC, Katzan I, Kernan WN, Mitchell PH, Ovbiagele B, Palesch YY, Sacco RL, Schwamm LH, Wassertheil-Smoller S, Turan TN, Wentworth D. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2011;42:227-276.
20. Pia Sormani M. The Will Rogers phenomenon: the effect of different diagnostic criteria. J Neurol Sci. 2009;287 Suppl 1:S46-49.
