Current status and future treatments.

Safa Younis

Mohammad Wasay
by Mohammad Wasay, MD, FRCP, FAAN, and Safa Younis, MBBS
Tuberculosis (TB) carries a huge burden around the globe. Approximately 25% of the global population is a carrier of the mycobacterium tuberculosis bacterium. About 5%-10% of the individuals in that group will develop tuberculosis during their lifetime.1
Although pulmonary TB is the primary form, extrapulmonary TB (EPTB) accounts for 15% of cases.2 Central nervous system tuberculosis (CNS-TB) is a severe type of tuberculosis, and it accounts for 1%-2% of TB cases worldwide.3 CNS-TB is more common in children and is associated with a high morbidity and mortality, especially in children under 5 years of age and patients under immunosuppression.4,5 With about 10 million new TB patients diagnosed each year, it is estimated that around 100,000 new cases of CNS-TB occurred in 2019.5
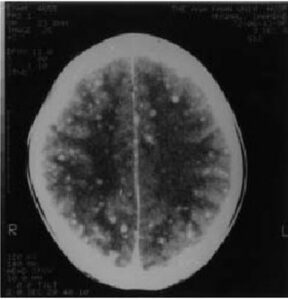
Figure 1. Post-contrast CT scan in axial plane showing multiple enhancing lesions in the brain. The diagnosis of TB was confirmed by CSF.
Tuberculous Meningitis
The most common type of CNS-TB is tuberculous meningitis (TBM) with an estimated prevalence of 2.11 per 100,000 people and mortality rates from 20%-50%. One-third of survivors with CNS-TB suffer long-term neurological disabilities such as cranial nerve palsies, hemiparesis, ophthalmoplegia, psychiatric disorders, and seizures. The morbidity and mortality rates of CNS-TB are associated with a country’s TB burden, Human Development Index (HDI), and the prevalence of HIV. Low- and middle-income countries are disproportionately affected.
Tuberculous meningitis is relatively rare and difficult to diagnose, therefore it often goes under-reported. TBM accounts for 5%-10% of all TB cases. It has a high morbidity and is responsible for 40% of deaths due to TB.8,9
TBM can cause severe complications like space-occupying tuberculomas and cerebral infarction.6 This results in a poor prognosis. The frequency of infarction in TBM has a wide range from 15%-27%. A greater occurrence is observed in young children who may be severely affected. Inflammatory basal exudate surrounding critical cerebral arteries like the circle of Willis and its branches can cause a periarteritis that is responsible for obliterative vasculitis and infarction.7 Infarction is a predictor of long-term disability in TBM patients.8
Tuberculous Myelitis
Tuberculous myelitis affects up to 3% of patients with TB. This is typically due to hematogenous spread of mycobacterium tuberculosis and can involve the spinal cord, roots, or spinal meninges. In developing countries, spinal TB is one of the most common causes of paraparesis.
In a study that took place in Aga Khan University Hospital in Pakistan, 20 patients with TB myelitis were identified through the ICD-9 coding system but only 10 fulfilled the inclusion criteria. The most prevalent symptoms observed in these patients upon presentation included:
- fever (70%)
- paraplegia (60%)
- paraparesis (30%)
- urinary retention (50%)
- bowel incontinence (30%)
- urinary incontinence (20%)
- monoparesis (10%)
Spinal tuberculoma or TB myelitis can occur after initiating antitubercular therapy for tuberculous meningitis or systemic TB. This phenomenon is called a paradoxical response.9 The paradoxical response to antitubercular therapy (ATT) typically occurs around two weeks into treatment. It may involve a worsening of existing tuberculous lesions or the appearance of new lesions in patients who initially showed improvement with ATT. Up to 10% of patients with CNS-TB may experience this with a higher rate of up to 30% with those with HIV.10
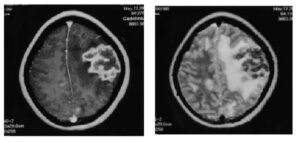
Figure 2. Left: Post-contrast T1-weighted MRI in axial plane showing a multilobular enhancing lesion in left frontal lobe. Right: T2-weighted MRI in axial plane showing multilobular mass with surrounding edema. The diagnosis of TB was confirmed by biopsy and histopathology.
Imaging and Diagnosis
Imaging plays a crucial role in diagnosing CNS-TB and its complications, as well as monitoring treatment response. Contrast-enhanced magnetic resonance imaging (MRI) is the preferred modality of choice due to its diagnostic accuracy. CNS-TB may closely resemble other neurological conditions, such as brain tumors. Thus, it is important for clinicians to have better understanding and familiarity of the imaging features of CNS-TB on computed tomography (CT) and MRI to aid in a quick and accurate diagnosis. CNS-TB can present in various ways on imaging, such as a diffuse form like basal exudative leptomeningitis, or localized forms like abscesses, tuberculomas, ventriculitis, or cerebritis. Meningitis (95%) and tuberculomas (2%) are the most common presentations.11
Radiomics is an evolving field of research focused on enhancing diagnostic precision by extracting quantitative data from clinical images. Magnetic resonance (MR) based radiomic features are gaining recognition in numerous intracranial pathologies, including tumors and neurodegenerative disorders. Studies suggest that certain MR textural parameters — including histogram skewness, gray-level co-occurrence matrix (GLCM) correlation, and neighboring gray-level dependence matrix (NGLDM) coarseness — hold promise as imaging biomarkers. Biomarkers such as these have the potential to predict response to treatment in patients with intracranial tuberculomas.12
Treatment and Long-Term Care
If clinical suspicion arises from imaging, treatment typically comprises of antitubercular therapy. There is a four-drug regimen (ethambutol, isoniazid, pyrazinamide, rifampin) supplemented with a corticosteroid that may reduce morbidity and mortality. However, drug resistance, immune reconstitution inflammatory syndrome (IRIS), and HIV coinfection can significantly complicate the diagnosis and management of CNS-TB.13
According to the British Infection Society, there can be a multiphase treatment therapy for tuberculosis. The initial phase, lasting 2-3 months, involves a combination of isoniazid, pyrazinamide, and rifampin, along with either ethambutol, fluoroquinolone, or a streptomycin. This is followed by a consolidation phase of up to 12 months, during which isoniazid and rifampin are continued. In some cases, the total treatment duration may be extended to 18 months.
For drug-resistant tuberculosis, treatment should be guided by specific resistance patterns and relevant guidelines. Throughout treatment, close monitoring of blood counts, liver function, and kidney function is essential as first-line antituberculosis drugs can cause hematologic abnormalities and organ damage. Vigilance and close monitoring for adverse drug reactions and prompt management are also crucial aspects of care.14
The success of CNS-TB treatment is highly contingent on timely intervention. Several factors influence the prognosis, with the clinical stage at initial presentation being the most important determinant. If left untreated or unrecognized, this disease can unfortunately lead to fatality within five to eight weeks of the onset of symptoms.15 •
End TB Strategy
To raise the profile of neurological disorders globally, the World Federation of Neurology (WFN) leverages its position as a WHO non-state actor and a non-governmental organization in consultative status with the UN Economic and Social Counsel (ECOSOC). The WFN commends the progress of the End TB Strategy, adopted by the World Health Assembly in 2014 as part of the Sustainable Development Goals (SDGs), and has taken the opportunity to intervene on several occasions to bring attention to the neurological complications of tuberculosis.
A written statement was submitted during the September 2023 SDG Summit in New York, highlighting the need for collaboration among multiple stakeholders and equitable access to health care to ensure the success of the End TB Strategy. The role of neurologists is crucial for the diagnosis, treatment, and prevention of the dangerous neurological complications of TB, including tuberculous meningitis. In May 2024, the WFN delegation had the privilege to address the World Health Assembly in Geneva and reaffirm the interconnection between decreasing the burden of tuberculosis and neurological health.
—Ksenia Pochigewa, Alla Guekht, Wolfgang Grisold.
Mohammad Wasay is Alicharan Endowed professor of neurology at Aga Khan University, past president of the Pakistan Society of Neurology and Pakistan Stroke Society, president of the Neurology Awareness and Research Foundation, trustee and chair of the Specialty Groups Committee of World Federation of Neurology (WFN), secretary of the Environmental Neurology specialty group of WFN, member of the Global Policy Committee of the World Stroke Organization (WSO), and editor of the Pakistan Journal of Neurological Sciences. Dr. Safa Younis completed her bachelor’s in medicine and surgery (MBBS) from Ziauddin Medical University, and is actively involved in raising awareness and promoting brain wellness within the community.
References
1. Dian S, Ganiem AR, van Laarhoven A. Central nervous system tuberculosis. Current Opinion in Neurology. 2021 Mar 3;34(3):396–402. doi:10.1097/wco.0000000000000920.
2. Navarro-Flores A, Fernandez-Chinguel JE, Pacheco-Barrios N, Soriano-Moreno DR, Pacheco-Barrios K. Global morbidity and mortality of central nervous system tuberculosis: A systematic review and meta-analysis. Journal of Neurology. 2022 Mar 15;269(7):3482–94. doi:10.1007/s00415-022-11052-8.
3. Pant A, Farrokhi F, Gyawali P, Yekuno K, Shah O, Singh S, et al. Global research trends in central nervous system tuberculosis — a bibliometric analysis. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases. 2024 Feb;34:100414. doi:10.1016/j.jctube.2024.100414.
4. Dian S, Ganiem AR, van Laarhoven A. Central nervous system tuberculosis. Current Opinion in Neurology. 2021 Mar 3;34(3):396–402. doi:10.1097/wco.0000000000000920.
5. Pant A, Farrokhi F, Gyawali P, Yekuno K, Shah O, Singh S, et al. Global research trends in central nervous system tuberculosis — a bibliometric analysis. Journal of Clinical Tuberculosis and Other Mycobacterial Diseases. 2024 Feb;34:100414. doi:10.1016/j.jctube.2024.100414.
6. Wasay M, Farooq S, Khowaja ZA, Bawa ZA, Ali SM, Awan S, et al. Cerebral infarction and Tuberculoma in central nervous system tuberculosis: Frequency and prognostic implications. Journal of Neurology, Neurosurgery & Psychiatry. 2014 Mar 12;85(11):1260–4. doi:10.1136/jnnp-2013-307178.
7. Taqui AM, Wasay M. Cerebral Infarction in Tuberculous Meningitis. Pakistan Journal of Neurological Sciences. 2011 Jan;6(1):25–9.
8. Wasay M, Khan M, Farooq S, Khowaja ZA, Bawa ZA, Mansoor Ali S, et al. Frequency and impact of cerebral infarctions in patients with tuberculous meningitis. Stroke. 2018 Oct;49(10):2288–93. doi:10.1161/strokeaha.118.021301.
9. Wasay M, Arif H, Khealani B, Ahsan H. Neuroimaging of tuberculous myelitis: Analysis of ten cases and review of literature. Journal of Neuroimaging. 2006 Jun 28;16(3):197–205. doi:10.1111/j.1552-6569.2006.00032.
10. Wasay M. Central nervous system tuberculosis and paradoxical response. Southern Medical Journal. 2006 Apr;99(4):331–2. doi:10.1097/01.smj.0000209231.88651.07.
11. Azeemuddin M, Alvi A, Sayani R, Khan MK, Farooq S, Beg MA, et al. Neuroimaging findings in tuberculosis: A single‐center experience in 559 cases. Journal of Neuroimaging. 2019 May 21;29(5):657–68. doi:10.1111/jon.12627.
12. Muhammad A, Khan S, Mohammad W, Muhammad A, Shoukat A, Khan H. Mr textural features (RADIOMICS) for predicting response to treatment in patients with intracranial tuberculoma: A retrospective cross-sectional study. Pakistan Journal of Neurological Sciences. 2023 Feb 5;17(03). doi:10.56310/pjns.v17i03.176.
13. Gupta M, Tobin EH, Munakomi S. CNS Tuberculosis. [Updated 2024 May 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585138/.
14. Chen W, Huang L, Tang Q, Wang S, Hu C, Zhang X. Progress on diagnosis and treatment of central nervous system tuberculosis [Internet]. Radiology of Infectious Diseases [Radiol Infect Dis]. 2020 [cited 2020 Aug 10];7(4):160-169. https://doi.org/10.1016/j.jrid.2020.07.005.
15. Gupta M, Tobin EH, Munakomi S. CNS Tuberculosis. [Updated 2024 May 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585138/.
