By Meah Mingyang Gao, MD; Russell Rasquinha, MD, MASc; Manav V. Vyas, MBBS, MSc; Mary Jane Lim Fat, MD; Yuri Kiryanov, MD; Clecio Godeiro, MD, PhD; Fernando Morgadinho Coelho, MD, PhD; Dalia Rotstein, MD, MPH, FRCPC; Tim Patterson; and Morris Freedman, MD, FRCP
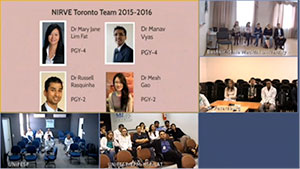
A screenshot of NIRVE rounds in September 2015 — First round for the new cycle (2015-16) where all sites introduce themselves. Top left: Slides being presented at the NIRVE rounds from Toronto. Top right: Trainees and staff at Ufa, Russia; and below, trainees and staff at St Petersburg, Russia. Bottom left: Natal, Brazil, and Sà£o Paulo, Brazil.
The 2013 WFN neurology training survey highlighted great variability in neurology training programs across the world.1 Neurology trainees are interested in international clinical experiences, but are often constrained by limited flexible time as well as financial, educational or logistical support.2 With the advent of modern technology, 95 percent of current international neurology trainees have reliable Internet access.1 Video-conferenced medical rounds are a new and proven way to supplement medical education across distances and may represent a sustainable solution to global peer learning.3,4
The Neurology International Residents Videoconference and Exchange (NIRVE) is a resident initiative sponsored by the Peter A. Silverman Global e-Health Program, the Canada International Scientific Exchange Program (CISEPO) and the Baycrest Center for Geriatric Care in Toronto. In 2009, Dr. Dalia Rotstein, a former neurology resident and now faculty member at the University of Toronto, established NIRVE with the vision to connect neurology residents across various geographical sites. NIRVE was modeled on the International Behavioral Neurology Videoconference Rounds.5
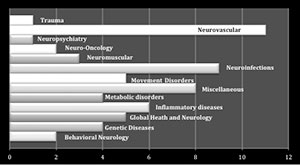
Figure 1. 61 distinct round topics (main case and image challenge) at 45 NIRVE rounds
NIRVE was designed to develop leadership skills and create opportunities for residents at all levels to participate in medical education and peer learning, raise awareness of global health concepts in neurology, increase resident advocacy of global health issues, enhance international and national collaboration among neurology residents and act as a gateway for organizing on-site exchanges.
The participating international sites on a rotating basis host the rounds every first Thursday morning of the month. Residents from the host site present a neurology case through videoconferencing technologies, and neurology resident moderators encourage the audience to actively engage in discussions and exchange opinions in real time.
Since its inception, NIRVE has continued to grow and expand. Neurology residents, fellows and faculty from Toronto with international contacts or affiliations initially recruited partner sites. For example, Olga Finlayson, a former University of Toronto neurology resident, helped establish a lasting collaboration and later clinical exchange with the First State Pavlov University in St. Petersburg, Russia. Our current partner sites include Natal, Brazil; Sà£o Paulo, Brazil; Grenoble, France; Jos, Nigeria; and Ufa, Russia. Participation is free and any site in the world with videoconference technology is welcome to join NIRVE as an equal partner.
Methods

Table 1. Results for educational value of NIRVE rounds in 2015 (N = 25)
The rounds start at 8 a.m. Eastern time, with a 30-minute case presentation and a 15-minute “image challenge” focused on a radiological or pathological diagnosis, with accompanying neuro-images. The rounds include sufficient time to engage residents in discussions involving diagnostic steps and therapeutic management across the different international sites. The current video-conferencing equipment (H.323/SIP connection protocol) is free within Ontario. International sites connect through a video conference MCU or bridge (Resolve Collaboration) at an hourly rate of slightly more than $35 per site (sponsored by the Peter A. Silverman Global e-Health Program, CISEPO and Baycrest Center for Geriatric Care).5 As of 2015, webcasting with password protection has been implemented using the Ontario Telemedicine Network, allowing any resident with Internet to connect to our rounds.6
As a resident-led initiative, NIRVE values all input from its participants and actively seeks feedback to further improve the program and curriculum to cater to participant needs. In 2015, a formal survey was distributed to all NIRVE participants and site directors from 2014-2015. The questionnaire consisted of four parts: demographic information, questions on the main case presentation, questions on the image challenge and exchange participation. The survey assessed both qualitative and quantitative responses from the participants and was administered using Survey Monkey®.
Results
More than 100 trainees from 10 different sites have attended NIRVE rounds since its inception. Figure 1 shows the categories and number of presentations in each category that have been covered at the NIRVE rounds, with neurovascular and neuroinfectious diseases being the two most common.
Twenty-seven, or 60 percent, of the 45 trainees across four different sites participated in the survey. The average age of these trainees between the ages of 24 to 53 was 29.4 years, and 16, or 60 percent of trainees, were females. While most were neurology residents at different levels of training, two sub-specialty fellows, one postdoctoral fellow and two PhD students also participated in the survey. Slightly more than 66 percent of trainees identified languages other than English as the language of instruction in their medical training. Of the 25 residents surveyed, 91.6 percent thought that the rounds were relevant to their level of training, 95.8 percent identified that the rounds contributed to their existing knowledge and 87.5 percent agreed that the topics align with their academic interests (Table 1). Seventy-two percent of trainees were interested in presenting at the rounds in the future, and 80 percent indicated an interest in participating in a future clinical exchange program. Most trainees identified the case discussions as the most beneficial aspect of the rounds and suggestions were made to increase emphasis on global health topics and comparing and contrasting practices across the world.
Discussion
There are considerable variations in the occurrence and management of neurological conditions across the world. As neurology trainees prepare for their future careers in an increasingly globalized world, providing early exposure to a variety of cases and management strategies can be challenging. NIRVE provides an opportunity to fill this gap while fostering a platform for potential collaborations.
Over the past years, NIRVE has encountered considerable challenges limiting its expansion. The difference in time zones across countries, various costs associated with room rental and equipment purchase for some international sites, and English as the main language for the rounds have limited the number of trainees we have been able to engage. Looking to the future, creating a bigger role for webcasting, and password-protected archived webcasts could be a more cost-effective strategy to expand our reach. However, increased connectivity may come at the price of reduced real-time interaction. Finally, an on-site clinical exchange is planned for May 2016 in Toronto, including participants from Brazil, Canada and Russia.
Conclusion
Despite challenges including technological, logistical and language-related constraints, NIRVE rounds continue to supplement resident learning across different geographical, political and cultural backgrounds. We welcome residents and fellows from other programs to contact us at nirve.utoronto@gmail.com for more information about NIRVE or to participate in NIRVE. We are happy to provide further information on some technical requirements and further details.
References
- Steck A, Struhal W, Sergay SM, Grisold W and the Education Committee World Federation of Neurology. The global perspective on neurology training: the World Federation of Neurology survey. J Neurol Sci. 2013; 334(1-2):30-47
- Lyons JL, Coleman ME, Engstrom JW, Mateen FJ. International electives in neurology training: a survey of US and Canadian program directors. Neurology. 2014; 82(2): 119-25
- Ali J, Sorvari A, Camera S, Kinach M, Mohammed S, Pandya A. Telemedicine as a potential medium for teaching the Advanced Trauma Life Support (ATLS) course. Journal of Surgical Education. 2013; 70(2): 258-264
- Ricci MA, Caputo MP, Callas PW, and Gagne M. The use of Telemedicine for delivering continuing medical education in rural communities. Telemedicine and e-Health. 2005; 11(2): 124-129
- Patterson T, Gouider R and Freedman M. Canada, Tunisia Link up for Long Distance Education. World Neurology. 2012; 27(1): 8
- Brown EM. The Ontario Telemedicine Network: a case report. Telemed J E Health. 2013; 19(5):373-6







 1) Ivana Vodopivec, et al. provides a glimpse of the heterogeneity of patients with Susac syndrome. Susac syndrome is a rare disease, which is usually characterized by a triad of encephalopathy, visual disturbances and hearing loss attributed to a pauci-inflammatory vasculopathy of the brain, eye and inner ear. However, at initial presentation, none of the five patients in this case series demonstrated the complete triad, and diagnosis was difficult and delayed. The authors provide two important conclusions: a) Microinfarcts were noted on MRI diffusion weighted imaging (DWI) of the brain, as well as branch retinal artery occlusions and vessel wall hyperfluorescence on fluorescein angiography in all patients with acute encephalopathy, and b) glucocorticoid and IVIg treatments were insufficient in halting the disease in patients with severe encephalopathy. Additional immunosuppressive treatment was required.
1) Ivana Vodopivec, et al. provides a glimpse of the heterogeneity of patients with Susac syndrome. Susac syndrome is a rare disease, which is usually characterized by a triad of encephalopathy, visual disturbances and hearing loss attributed to a pauci-inflammatory vasculopathy of the brain, eye and inner ear. However, at initial presentation, none of the five patients in this case series demonstrated the complete triad, and diagnosis was difficult and delayed. The authors provide two important conclusions: a) Microinfarcts were noted on MRI diffusion weighted imaging (DWI) of the brain, as well as branch retinal artery occlusions and vessel wall hyperfluorescence on fluorescein angiography in all patients with acute encephalopathy, and b) glucocorticoid and IVIg treatments were insufficient in halting the disease in patients with severe encephalopathy. Additional immunosuppressive treatment was required.


 Although ancient Egyptians were the first to describe the brain, the services that are provided to patients with disorders of the brain and the number of trained neurologists in Arab and African countries is at best centralized in large cities and at worst nonexistent.
Although ancient Egyptians were the first to describe the brain, the services that are provided to patients with disorders of the brain and the number of trained neurologists in Arab and African countries is at best centralized in large cities and at worst nonexistent.
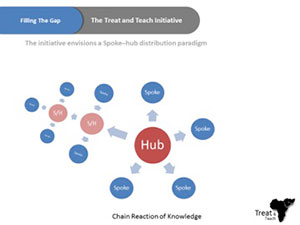 For the aforementioned reasons, Ain Shams University has been endorsing an initiative called Treat and Teach, which is designed to develop short- and intermediate-term strategies to reduce the gap in the number of trained neurologists and the deficiency of neurology education programs in Africa. We are trying to complement the current efforts to improve neurology education in Africa with an initiative that has a mix of online education and on-site clinical training, while working on establishing medical services that may include a stroke unit, memory clinic, neurorehabilitation units, or a neurology department. Master degrees will be given from Ain Shams University, Cairo, and work will be done to establish local master degrees in rural centers. This could lead to national neuroscience services run by local providers.
For the aforementioned reasons, Ain Shams University has been endorsing an initiative called Treat and Teach, which is designed to develop short- and intermediate-term strategies to reduce the gap in the number of trained neurologists and the deficiency of neurology education programs in Africa. We are trying to complement the current efforts to improve neurology education in Africa with an initiative that has a mix of online education and on-site clinical training, while working on establishing medical services that may include a stroke unit, memory clinic, neurorehabilitation units, or a neurology department. Master degrees will be given from Ain Shams University, Cairo, and work will be done to establish local master degrees in rural centers. This could lead to national neuroscience services run by local providers.