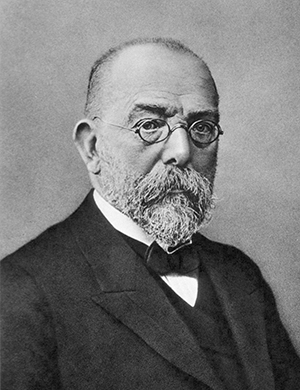
By Nguyen Huu Cong

Nguyen Huu Cong
Through the aid of the World Federation of Neurology (WFN) and the American Academy of Neurology (AAN), the continuum courses have been carried out for many years in Vietnam. The courses are conducted one to two times a year, with the topics chosen by members of the executive committee of the Ho Chi Minh City Neurological Association, based on the issues delivered annually by the WFN and AAN. These courses are usually organized in Ho Chi Minh City, the largest city in Southern Vietnam. On May 6, the course took place for the first time outside Ho Chi Minh City in the Mekong Delta.
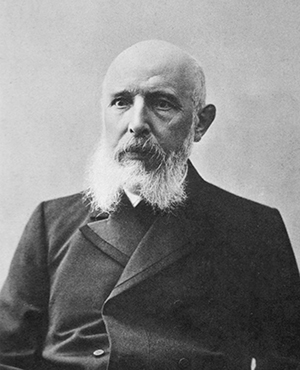
The Tien Giang Neurological Association (TNA) was founded one year ago in My Tho, a beautiful small town in the Mekong Delta and the capital of Tien Giang Province. It now has 60 members. Most of them are neurologists from the surrounding provinces in the Mekong Delta, but some are internists working in rural areas without neurologists. Dr Nguyen Van Thanh, chief of the department of neurology at Tien Giang Hospital and president of the Tien Giang Neurological Association, is actively working and running the association.
The Vietnamese Association of Neurology and the Ho Chi Minh City Neurological Association have been assisting the TNA by sending our experts to attend lectures there. This year’s continuum course, held at Tien Giang General Hospital, covered the topics of epilepsy, as presented in Continuum: Lifelong Learning in Neurology, Vol. 19, Issue 3, June 2013. The lecturers were Prof. Pierre Jallon, former professor of neurology at the University of Geneva; Le Van Tuan, MD, PhD; and Tran Quang Tuyen MD, from the Ho Chi Minh City Neurological Association. The lectures focused on these articles:
- The 2010 Revised Classification of Seizures and Epilepsy
- Antiepileptic Drug Treatment: New Drugs and New Strategies
- EEG and Epilepsy Monitoring
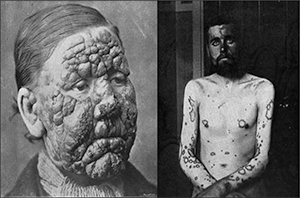
Prof. Pierre Jallon presented the old and new definitions, compared previous to revised classifications and analyzed the advantages of new terms and concepts and their limitations. Then the professor also talked about the differential diagnosis, especially in difficult cases from the features of syncope convulsions, hypoglycemia and psychogenic nonepileptic seizure. Subsequently, Dr. Le Van Tuan introduced the article, “Antiepileptic Drug Treatment: New Drugs and New Strategies,” speaking about the targets of epilepsy treatment, classical AEDs and newer medications available in our country. He also showed how to select antiepileptic drugs appropriate for each types of seizure. The topic of AED treatment fascinated all of the attendees, and they started a fervent conversation with the lecturer. Dr. Tran Quang Tuyen introduced the usefulness of video EEG in supposing epilepsy diagnosis. On this occasion, Drs. Le Van Tuan Tran Quang Tuyén, took turns to report on the situation of using EEG in Vietnam for epilepsy monitoring. Once again, many questions related to clinical practice were asked of the lecturers. After the presentations, attendees were encouraged to discuss the contents of the articles, “Patient Management Problem” and “Patient Management Problem — Preferred Responses.”
The discussion lasted past the fixed hours. At the end of the course, Dr. Nguyen Van Thanh, president of the TNA, expressed the gratitude of the Tien Giang Association members to the lecturers, AAN and WFN. The participants showed their gratitude in kind and suggested similar educational courses in the Mekong Delta in the future.
The CME course with Continuum — Lifelong Learning in Neurology has contributed to improving the knowledge of epilepsy in our neurologists in Tien Giang and the surrounding provinces.
The issues of the Continuum: Lifelong Learning in Neurology, with articles written by experts from the American Academy of Neurology, are useful for our neurologists, especially young members of our associations in Vietnam. We are planning to organize one additional course in August 2015 on “Peripheral Nervous System Disorders.” We believe that afterward we will continue to have the assistance of the World Federation of Neurology.